Sex after prostate cancer
Rediscovering Intimacy After Prostate Cancer: Your Journey to Healing and Connection
Life after prostate cancer treatment is not an end—it’s the beginning of a new chapter filled with opportunities for growth, healing, and deeper connections. For men aged 40 to 80, navigating changes in sexual health is a significant part of this journey. As part of our Urology Wellness Journey for Movember, we’re here to offer evidence-based insights and compassionate support to help you rediscover intimacy and embrace a fulfilling life post-treatment.
Understanding the Changes
Imagine setting out on a familiar path, only to find it has transformed in unexpected ways. Prostate cancer treatments save lives but can bring about changes in sexual function that may feel challenging. Recognizing and understanding these changes is the first empowering step toward healing.
Immediate Effects
It’s common for most men to experience some degree of erectile dysfunction (ED) after prostate cancer treatment, especially following surgery (radical prostatectomy) or radiation therapy. The extent and duration of ED can vary based on factors like the type of treatment, age, and overall health.
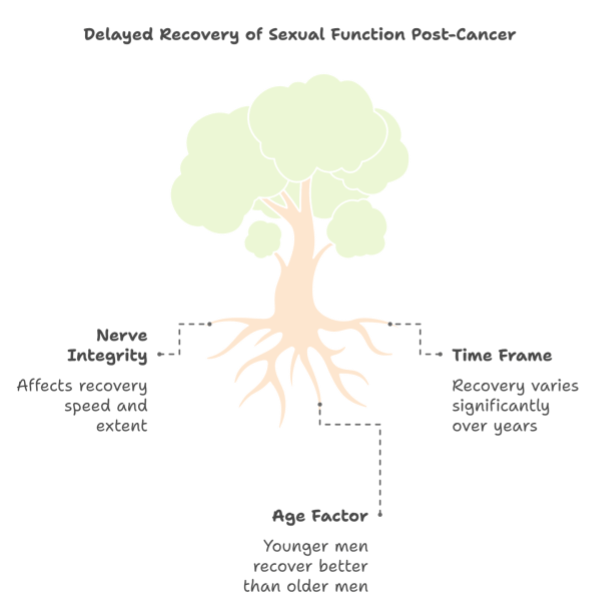
Recovery Timeline
Remember, healing is a deeply personal process, and recovery of sexual function takes time:
- Within One Year: Many men notice substantial improvement, especially if nerves were spared during treatment. About 40-50% regain their pre-treatment function within a year.
- Up to Two Years: Recovery can continue over two years, with approximately 30-60% regaining their previous level of function by the second year.
- Age Factor: Younger men often have better outcomes. For instance, men under 65 have a 59.3% potency rate after one year, compared to 31.3% for men over 75.
Enhancing Recovery – Strategies for Sexual Health
There are several proactive approaches to support the recovery of sexual function:
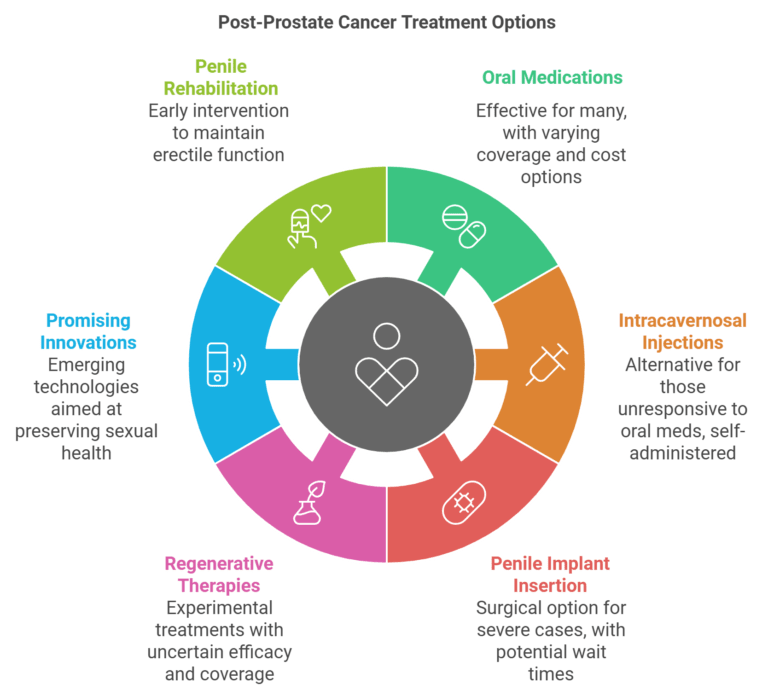
Medical Treatments
1- Oral Medications:
- Medications like sildenafil (Viagra), tadalafil (Cialis), and vardenafil (Levitra) can enhance blood flow.
- Effective for about 75% of men post-nerve-sparing prostatectomy or targeted radiation.
- Often covered by public health systems, but coverage varies by country and health plan.
- Generic versions are increasingly available, reducing costs.
2- Intracavernosal Injections:
- For men who don’t respond to oral medications.
- Involves injections of alprostadil or a combination of vasoactive drugs.
- Taught by a healthcare provider and self-administered at home.
- Coverage varies; some may pay out-of-pocket.
3- Penile Implant Insertion:
- Option for severe ED unresponsive to other treatments.
- Surgical insertion of a penile implant (prosthesis).
- Typically covered when deemed medically necessary, but waiting times can vary.
4- Regenerative Therapies:
- Experimental treatments like stem cell therapies or platelet-rich plasma (PRP) injections.
- Aim to regenerate nerve and tissue function.
- Not typically covered by public health systems; efficacy still under study.
5- Promising Innovations:
- Advanced imaging and precision-guided therapies minimize damage to erectile function.
- Emerging focal therapies and structure-sparing approaches offer hope for preserving sexual health.
- Gene therapy and tissue engineering are being explored for potential regeneration of erectile tissue.
6- Penile Rehabilitation:
- Includes regular use of oral medications, injections, or vacuum devices soon after treatment.
- Promotes blood flow and prevents long-term ED.
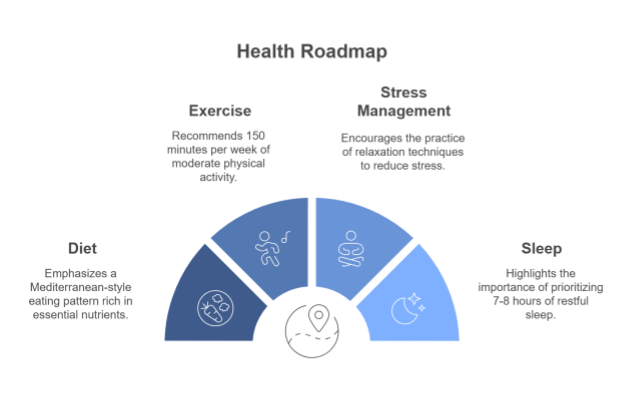
Lifestyle Modifications
1- Healthy Weight & Exercise:
- Regular physical activity and maintaining a healthy weight can positively impact erectile function.
2- Quit Smoking & Limit Alcohol:
- Smoking damages blood vessels.
- Excessive alcohol can interfere with sexual performance.
Nutritional Interventions
Fuel your body with nutritious choices to support overall health:
1- Increase Fruits and Vegetables:
- Rich in antioxidants; may help reduce cancer risk.
2- Incorporate Omega-3 Fatty Acids:
- Found in fish or plant sources; may have protective effects against prostate cancer.
3- Limit Refined Carbohydrates and Saturated Fats:
- Some studies suggest these may be associated with increased prostate cancer risk.
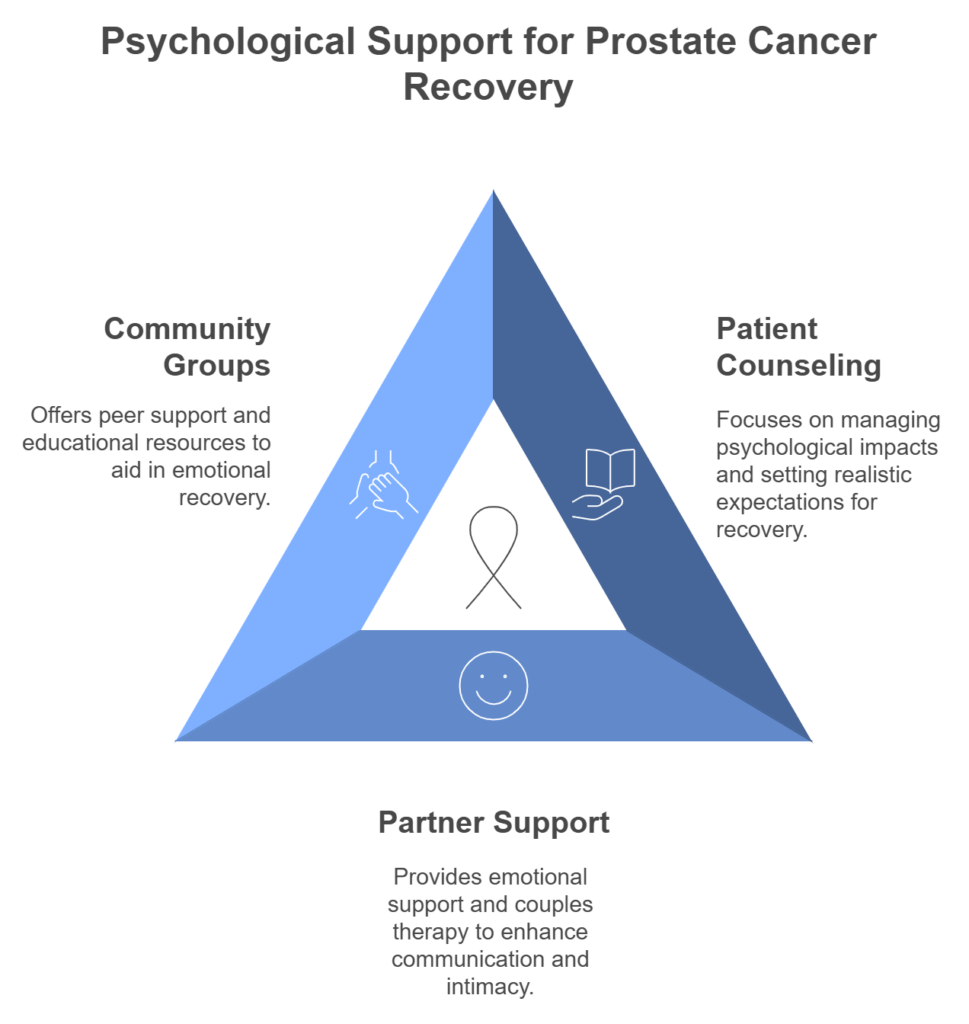
Psychological Support
Healing is not just physical; it’s emotional and psychological as well.
For Patients
- Psychosexual Counselling:
- Crucial for addressing body image, self-esteem, and emotional aspects of sexual recovery.
- Provides realistic recovery timelines and helps manage expectations.
For Partners
- Emotional Support:
- Individual counselling helps partners process their own feelings and concerns.
2. Couples Therapy:
- Joint sessions improve communication.
- Helps both partners adjust to changes in intimacy.
Community and Support Groups
You don’t have to navigate this journey alone.
- Peer Support:
- Groups like Us TOO International and the Prostate Cancer Foundation offer forums to share experiences and coping strategies.
2. Educational Resources:
Access up-to-date information on treatments and side effect management.
Real-Life Emotional Histories
Mark’s Story
Being diagnosed with prostate cancer under the age of 50 isn’t common, but that’s exactly what happened to Mark at 45. After noticing blood in his urine, he sought medical advice, leading to a prostate cancer diagnosis. The news was shocking and overwhelming, but Mark chose to face it head-on. Opting for surgery and subsequent radiotherapy and hormone therapy, he found strength in maintaining a positive attitude and continuing to work throughout his treatment.
During his journey, Mark met his future husband. Open and honest about his treatment and its side effects, like erectile dysfunction, he found unwavering support and understanding. “Sex is different now,” Mark says, “but there’s more to life than sex. If you’ve got a loving and strong relationship, that’s what life is about.” Together, they attend support groups, finding community and sharing experiences to help others navigate their own journeys.
John, 62
“After my surgery, I felt like less of a man. The support group helped me realize I wasn’t alone. Hearing others’ stories of recovery gave me hope and the courage to try different treatments.”
Maria, Partner of a Prostate Cancer Survivor
“The couples’ therapy sessions were eye-opening. We learned to communicate about intimacy in ways we never had before. It brought us closer despite the physical challenges.”
These stories highlight the transformative power of emotional support. They demonstrate how community and professional counselling can provide hope, reduce feelings of isolation, and improve quality of life for both patients and their partners.
Embracing Technology
- Telemedicine:
- Virtual consultations provide convenient follow-up care.
- Connect with others facing similar challenges from the comfort of your home.
Fertility Considerations
If you’re concerned about fertility:
- Sperm Banking:
- Consider preserving sperm before treatment if future fertility is a desire.
2. Fertility Consultations:
- Discuss options with a specialist to understand potential impacts and preservation methods.
Long-Term Monitoring and Follow-Up
- Regular Check-ups:
- Schedule periodic appointments to monitor sexual health and address new concerns.
- Be prepared to adapt your approach as your body continues to heal and change.
Conclusion
Embracing intimacy after prostate cancer is a journey of healing, connection, and rediscovery. With support from healthcare providers, partners, and resources like those offered by Movember, you can confidently navigate these changes and embrace a fulfilling life post-treatment. Remember, you’re not alone—resources are available to support you every step of the way.
Citations
- Nutrition and prostate cancer
- UCSF Health: Nutrition and prostate cancer
- Erectile dysfunction after prostate cancer treatment
- Prostate Cancer UK: Diet and physical activity
- National Cancer Institute: Prostate cancer supplements
- Cancer Research UK: Diet and prostate cancer
- Movember: Sex after prostate cancer
Remember, every journey is unique, but you don’t have to walk it alone. Reach out, stay connected, and keep moving forward.
