A Patient's Guide to Vasectomy: What You Need to Know
As a urologist, I’ve compiled this comprehensive guide to help you understand and prepare for your vasectomy procedure. This information is based on the most up-to-date research and clinical practices.
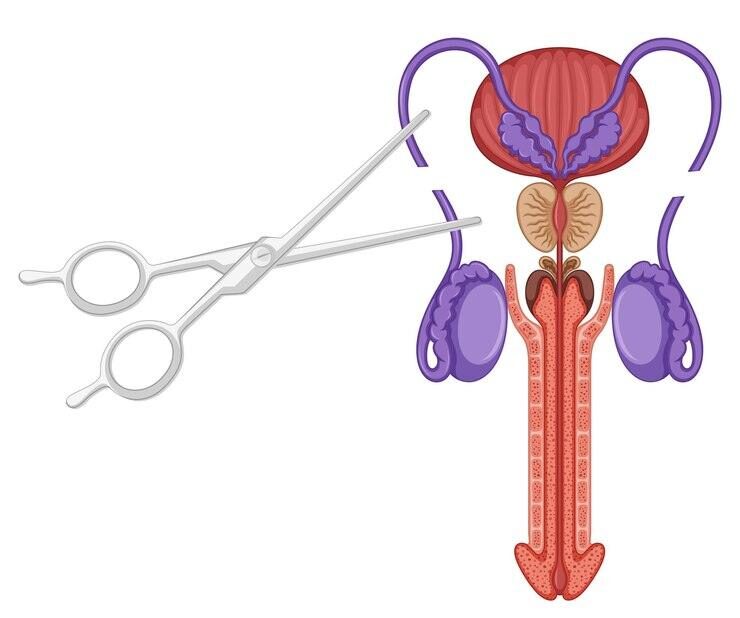
What is a Vasectomy?
A vasectomy is a minor surgical procedure that provides permanent male contraception. It involves cutting and sealing the vas deferens, the tubes that carry sperm from the testicles to the penis1. This prevents sperm from mixing with semen during ejaculation, effectively stopping pregnancy.
Effectiveness and Safety
Vasectomy is highly effective, with a success rate of over 99%. Recent data shows that the procedure is even safer than previously thought:
The risk of chronic scrotal pain is only about 0.2%, much lower than the previously quoted 5%10.
Infection rates are around 1.6%, lower than the 2-10% often cited10.
Hematoma (blood clot) rates are approximately 1.9%, also lower than previous estimates10.
Types of Vasectomy
There are two main types of vasectomy:
Conventional (Incision) Vasectomy:
Small incisions are made in the scrotum to access the vas deferens13.
No-Scalpel Vasectomy:
A minimally invasive technique using a small puncture instead of incisions1. Both methods are effective, but the no-scalpel approach may lead to fewer complications and faster recovery1.
Preparing for Your Vasectomy
To ensure the best possible outcome:
Shave your scrotum a few days before the procedure8.
Take a shower or bath on the morning of your vasectomy8.
Wear tight-fitting underwear on the day of surgery8.
Arrange for someone to drive you home after the procedure8.
The Procedure
A vasectomy is typically performed under local anesthesia and takes about 20-30 minutes17. You may feel some tugging or mild discomfort, but the area will be numb11.
Recovery and Aftercare
Most men recover quickly from a vasectomy. Here’s what to expect:
Some mild discomfort, bruising, and swelling for a few days6.
Use ice packs and wear supportive underwear to reduce swelling14.
Take over-the-counter pain relievers as needed14.
Avoid strenuous activity for about a week6.
You can usually return to work after 1-2 days3.
Important Considerations
Not Immediately Effective: Continue using other contraception until your doctor confirms the absence of sperm in your semen, usually after about 3 months and 20 ejaculations111.
Permanence: Consider vasectomy as a permanent procedure. While reversal is possible, it’s not always successful and is not typically covered by insurance3.
No Protection Against STIs: A vasectomy does not protect against sexually transmitted infections3.
Minimal Impact on Sexual Function: Vasectomy should not affect your sex drive, ability to have erections, or the sensation of orgasm7.
Potential Risks and Complications
While rare, be aware of these potential issues:
Infection (about 1.6% risk)10
Hematoma (about 1.9% risk)10
Chronic pain (about 0.2% risk)10
Sperm granuloma (a small, usually harmless lump)14
Failure rate of about 1 in 2,0001
Follow-up
It’s crucial to complete the post-vasectomy semen analysis as instructed by your doctor. This confirms the procedure’s success and that you can safely stop using other forms of contraception11.
Remember, a vasectomy is a significant decision. Discuss any concerns with your healthcare provider and ensure you’re comfortable with the choice before proceeding.
What are the most common complications after a vasectomy?
Not Immediately Effective: Continue using other contraception until your doctor confirms the absence of sperm in your semen, usually after about 3 months and 20 ejaculations111.
Permanence: Consider vasectomy as a permanent procedure. While reversal is possible, it’s not always successful and is not typically covered by insurance3.
No Protection Against STIs: A vasectomy does not protect against sexually transmitted infections3.
Minimal Impact on Sexual Function: Vasectomy should not affect your sex drive, ability to have erections, or the sensation of orgasm7.
Potential Risks and Complications
While rare, be aware of these potential issues:
Infection (about 1.6% risk)10
Hematoma (about 1.9% risk)10
Chronic pain (about 0.2% risk)10
Sperm granuloma (a small, usually harmless lump)14
Failure rate of about 1 in 2,0001
Follow-up
It’s crucial to complete the post-vasectomy semen analysis as instructed by your doctor. This confirms the procedure’s success and that you can safely stop using other forms of contraception11.
Remember, a vasectomy is a significant decision. Discuss any concerns with your healthcare provider and ensure you’re comfortable with the choice before proceeding.
Short-term Complications
Pain and Discomfort
Most men experience some level of pain and discomfort immediately following the procedure. This is typically mild and can be managed with over-the-counter pain relievers and supportive underwear15.
Bruising and Swelling
Bruising and swelling of the scrotum are common and usually resolve within a few days to a week after the procedure56.
Bleeding
Minor bleeding or a small hematoma (blood clot) can occur. Recent data suggests the risk of hematoma is around 1.9%, which is lower than previously thought13.
Infection
The risk of infection is relatively low, with recent estimates placing it at about 1.6%13. Most infections are mild and limited to the incision site.
Less Common Complications
Sperm Granuloma
These are small, usually harmless lumps that form at the end of the vas deferens. They occur in about 15-40% of men undergoing vasectomy but rarely cause symptoms12.
Post-Vasectomy Pain Syndrome (PVPS)
Chronic scrotal pain lasting more than three months occurs in about 1-2% of men who undergo vasectomy35. This is much lower than previously thought, with older estimates ranging from 1-14%3.
Epididymitis
Inflammation of the epididymis occurs in about 0.5-3% of cases12.
Rare Complications
Vasectomy Failure
The risk of vasectomy failure is very low, estimated at about 1 in 2,000 cases2.
Recanalization
In extremely rare cases, the vas deferens may reconnect, potentially restoring fertility6.
It’s important to note that serious long-term complications from vasectomy are rare, and the procedure is generally considered safe and effective. Most men recover quickly with minimal issues. However, as with any surgical procedure, it’s crucial to discuss potential risks and complications with your healthcare provider before deciding to undergo a vasectomy.
Are there any long-term side effects associated with vasectomy?
While vasectomy is generally considered a safe and effective form of permanent male contraception, there are some potential long-term side effects to be aware of. However, it’s important to note that serious long-term complications are rare.
Potential Long-Term Side Effects
Post-Vasectomy Pain Syndrome (PVPS)
PVPS is one of the most significant potential long-term side effects:
Occurs in approximately 1-2% of men who undergo vasectomy
Characterized by chronic scrotal pain lasting more than 3 months after the procedure
Can negatively impact quality of life in some cases
Treatment options include anti-inflammatory medications, nerve pain medications, and in rare cases, surgical intervention
Sperm Granulomas
Small, usually harmless lumps that form at the end of the vas deferens
Occur in about 15-40% of men who have had a vasectomy
Typically resolve on their own but may cause initial tenderness
Recanalization
Extremely rare occurrence where the vas deferens reconnect, potentially restoring fertility
Estimated to occur in less than 1% of cases
Debunked Long-Term Concerns
Several previously held concerns about long-term effects have been largely debunked by research:
Cancer Risk
Current evidence does not support an increased risk of prostate, testicular, or other cancers following vasectomy.
Cardiovascular Disease
No established link between vasectomy and increased risk of cardiovascular disease.
Autoimmune Diseases
Studies have not shown an increased risk of autoimmune diseases in men who have undergone vasectomy.
Sexual Function
Vasectomy does not typically affect sexual function, libido, or erectile function in the long term.
Are there any long-term side effects associated with vasectomy?
While vasectomy is generally considered a safe and effective form of permanent male contraception, there are some potential long-term side effects to be aware of. However, it’s important to note that serious long-term complications are rare.
Potential Long-Term Side Effects
Post-Vasectomy Pain Syndrome (PVPS)
PVPS is one of the most significant potential long-term side effects:
Occurs in approximately 1-2% of men who undergo vasectomy
Characterized by chronic scrotal pain lasting more than 3 months after the procedure
Can negatively impact quality of life in some cases
Treatment options include anti-inflammatory medications, nerve pain medications, and in rare cases, surgical intervention
Sperm Granulomas
Small, usually harmless lumps that form at the end of the vas deferens
Occur in about 15-40% of men who have had a vasectomy
Typically resolve on their own but may cause initial tenderness
Recanalization
Extremely rare occurrence where the vas deferens reconnect, potentially restoring fertility
Estimated to occur in less than 1% of cases
Debunked Long-Term Concerns
Several previously held concerns about long-term effects have been largely debunked by research:
Cancer Risk
Current evidence does not support an increased risk of prostate, testicular, or other cancers following vasectomy.
Cardiovascular Disease
No established link between vasectomy and increased risk of cardiovascular disease.
Autoimmune Diseases
Studies have not shown an increased risk of autoimmune diseases in men who have undergone vasectomy.
Sexual Function
Vasectomy does not typically affect sexual function, libido, or erectile function in the long term.
Other Considerations
Regret
While not a physical side effect, some men may experience long-term regret or uncertainty about their decision, particularly if life circumstances change.
Reversal Challenges
Although vasectomy reversal is possible, its success rate decreases over time and is not guaranteed.
In conclusion, while vasectomy is generally safe and effective, it’s crucial for men considering the procedure to discuss potential long-term effects with their healthcare provider to make an informed decision.
How common is chronic pain syndrome after a vasectomy?
Post-vasectomy pain syndrome (PVPS) is less common than previously thought, but still affects a significant number of men who undergo vasectomy. Based on the most recent and comprehensive data:
Incidence of PVPS
The incidence of post-vasectomy pain syndrome is approximately 5% (95% CI 3% to 8%)5. This means that about 1 in 20 men who undergo a vasectomy may experience chronic pain lasting more than three months after the procedure.
Factors Affecting Incidence
Several factors can influence the reported incidence of PVPS:
Vasectomy Technique: The incidence of post-vasectomy pain appears to be lower with the non-scalpel technique (7%) compared to the traditional scalpel technique (24%)5.
Definition of Chronic Pain: Studies vary in how they define chronic pain, which can affect reported rates.
How common is chronic pain syndrome after a vasectomy?
Post-vasectomy pain syndrome (PVPS) is less common than previously thought, but still affects a significant number of men who undergo vasectomy. Based on the most recent and comprehensive data:
Incidence of PVPS
The incidence of post-vasectomy pain syndrome is approximately 5% (95% CI 3% to 8%)5. This means that about 1 in 20 men who undergo a vasectomy may experience chronic pain lasting more than three months after the procedure.
Factors Affecting Incidence
Several factors can influence the reported incidence of PVPS:
Vasectomy Technique: The incidence of post-vasectomy pain appears to be lower with the non-scalpel technique (7%) compared to the traditional scalpel technique (24%)5.
Definition of Chronic Pain: Studies vary in how they define chronic pain, which can affect reported rates.
Follow-up Duration: Longer follow-up periods may reveal different incidence rates compared to short-term studies.
Severity of Pain
It’s important to note that not all cases of PVPS are severe or significantly impact quality of life:
About 1-2% of men who undergo vasectomy experience pain severe enough to seek medical attention or that interferes with quality of life12.
In one study, only 0.9% of men reported pain severe enough to affect quality of life 7 months after the procedure2.
Long-term Outcomes
Long-term studies on PVPS are limited, but available data suggests:
At 4.8 years post-vasectomy, 2.2% of men reported chronic scrotal pain severe enough to impact quality of life1.
In a comparative study with 3.9 years of follow-up, 6.0% of vasectomized men sought medical attention for testicular pain, compared to 2.0% of non-vasectomized men2.
While PVPS is a real concern for men considering vasectomy, it’s important to note that the vast majority of men who undergo the procedure do not experience chronic pain. However, patients should be counseled about this potential complication before deciding to proceed with a vasectomy.
Are there any preventive measures to avoid chronic pain syndrome after a vasectomy?
While post-vasectomy pain syndrome (PVPS) is relatively rare, there are several preventive measures that can be taken to minimize the risk of developing chronic pain after a vasectomy:
Choose an Experienced Surgeon
Selecting a skilled and experienced urologist to perform the vasectomy can reduce the risk of surgical complications that may lead to chronic pain.
Opt for Minimally Invasive Techniques
The no-scalpel vasectomy technique has been associated with a lower incidence of post-vasectomy pain compared to the traditional scalpel technique (7% vs. 24%)1.
Follow Post-Operative Instructions
Adhering to your surgeon’s aftercare guidelines is crucial:
Rest and avoid strenuous activities for about a week
Use ice packs on the scrotum intermittently for 24-48 hours
Wear supportive underwear or an athletic supporter for 1-2 weeks
Manage Early Pain and Inflammation
Take prescribed or over-the-counter pain medications as directed
Use non-steroidal anti-inflammatory drugs (NSAIDs) for 2-4 weeks if recommended
Gradual Return to Activities
Slowly resume normal activities and avoid heavy lifting for 5-7 days to reduce the risk of complications like scrotal hematoma5.
Attend Follow-up Appointments
Keep all scheduled follow-up appointments to ensure proper healing and address any concerns early.
Be Aware of Warning Signs
Seek medical attention promptly if you experience unusual pain, swelling, or signs of infection.
While these measures can help reduce the risk of PVPS, it’s important to note that some factors contributing to chronic pain may not be preventable. Always discuss your concerns with your healthcare provider before the procedure to ensure you fully understand the risks and potential complications.
Can diet or supplements help reduce the risk of chronic pain after a vasectomy?
While there is no specific diet or supplement regimen proven to directly prevent chronic pain after a vasectomy, certain nutritional approaches may help support overall healing and potentially reduce the risk of complications.
Here are some dietary and supplement strategies that could be beneficial:
Anti-Inflammatory Diet
Adopting an anti-inflammatory diet may help reduce inflammation and support healing:
Increase intake of fruits, vegetables, whole grains, and healthy fats like olive oil
Reduce consumption of processed foods, sugar, and unhealthy fats
Include foods rich in omega-3 fatty acids, such as fish, flaxseeds, and walnuts
Key Nutrients for Healing
Ensuring adequate intake of certain nutrients can support the body’s healing processes:
Vitamin C
Essential for collagen formation and tissue repair
Found in citrus fruits, berries, and leafy greens
Vitamin A
Aids in cell development and collagen formation
Sources include sweet potatoes, carrots, and spinach
Vitamin E
Acts as an antioxidant and supports immune function
Found in nuts, seeds, and vegetable oils
B-Complex Vitamins
Support energy production and red blood cell formation
Sources include whole grains, legumes, and lean meats
Hydration
Adequate water intake is crucial for healing and can help reduce pain sensitivity.
Supplements
While evidence is limited, some supplements may offer potential benefits:
Omega-3 fatty acids: May help reduce inflammation
Curcumin: Has anti-inflammatory properties
Vitamin D: Supports immune function and may help with pain management
It’s important to note that while these dietary approaches and supplements may support overall health and healing, they are not guaranteed to prevent chronic pain after a vasectomy. Always consult with a healthcare provider before starting any new supplement regimen, especially in the context of surgery recovery.

