Calm, evidence-based assessment. Clear diagnosis. And the right treatment matched to the actual cause—not guesswork.
Is this page for you?
This page is for you if: You're experiencing persistent difficulty getting or keeping erections firm enough for satisfying sex, and you want to understand why it's happening and what actually works—without hype, shame, or one-size-fits-all solutions.
This page is not for you if: You're looking for a quick prescription without assessment, or you believe ED is always "just psychological" or "just physical". ED is rarely that simple—and the best outcomes come from proper diagnosis, not guessing.
Erectile dysfunction (ED) is common—and it can feel intensely personal. Some men notice a sudden change; others feel things slowly drift over months or years. Either way, the first questions are usually the same:
- Why is this happening to me?
- Is it psychological or physical?
- Is this "normal" or a sign of something wrong?
- Am I broken—getting old—ill?
You're not alone in thinking that way. And you don't need to "power through it" quietly.
I'm Mr Ollandini, Consultant Urological Surgeon in London. My job is to help you understand what's driving your erectile dysfunction and guide you to the right pathway—without judgement, hype, or guesswork.
ED is not one condition. It's a symptom with different causes—and different solutions. Many men can improve with the right assessment and matched treatment.
Common pathways
How most men start
Understanding what's driving your ED
For many men, the first step is clarifying whether erectile dysfunction is mainly physical, psychological, or a mix—before choosing any test or treatment.
Start with a clinician-led assessment
A detailed history, examination, and targeted blood tests often point us in the right direction. Many men improve with correct first-line treatment.
Objective data when it changes decisions
When symptoms persist or treatment trials fail, investigations like penile Doppler ultrasound can help—so we avoid treating the wrong mechanism.
When to seek urgent help
If you have chest pain, severe breathlessness, fainting, or symptoms of stroke, seek urgent medical help. Erectile dysfunction can sometimes sit alongside cardiovascular risk.
On this page
What ED is (and what it isn't)
Erectile dysfunction means a persistent difficulty getting or keeping an erection firm enough for sex that's satisfactory for you (and, if relevant, your partner). It doesn't mean "zero erections ever". It doesn't automatically mean "low testosterone". And it doesn't automatically mean "it's all in your head".
Occasional difficulty can happen to anyone—fatigue, stress, alcohol, distraction, conflict. Erectile dysfunction is the pattern that keeps repeating.
A quick normaliser (that still takes you seriously)
Why erectile dysfunction happens
Most erectile dysfunction is multifactorial. You can have a physical driver and a psychological amplifier—and both deserve attention. The goal is not to "pick a team". The goal is to build a plan that works.
What we assess
Common drivers we look for
Blood flow (vascular erectile dysfunction)
Reduced inflow (arterial issues) and/or poor trapping of blood (veno-occlusive dysfunction). Risk factors include smoking, diabetes, high blood pressure, and high cholesterol.
Nerves (neurogenic ED)
Diabetes, pelvic surgery, spinal issues, and some neurological conditions can disrupt signalling.
Hormones (hormonal erectile dysfunction)
Low testosterone can reduce libido and contribute to ED in some men—but it's not the default explanation. Blood tests matter.
Medication & substances
Some antidepressants, blood pressure tablets, and other medications can contribute to erectile dysfunction. Alcohol and recreational drugs can as well.
Psychological & relational factors
Performance anxiety, stress, depression, porn-related arousal mismatch, and relationship strain can all play a role. This is physiology: your brain is part of the sexual response.
Penile structure (structural ED)
Pain, curvature, or Peyronie's disease can make erections unreliable or less satisfying.
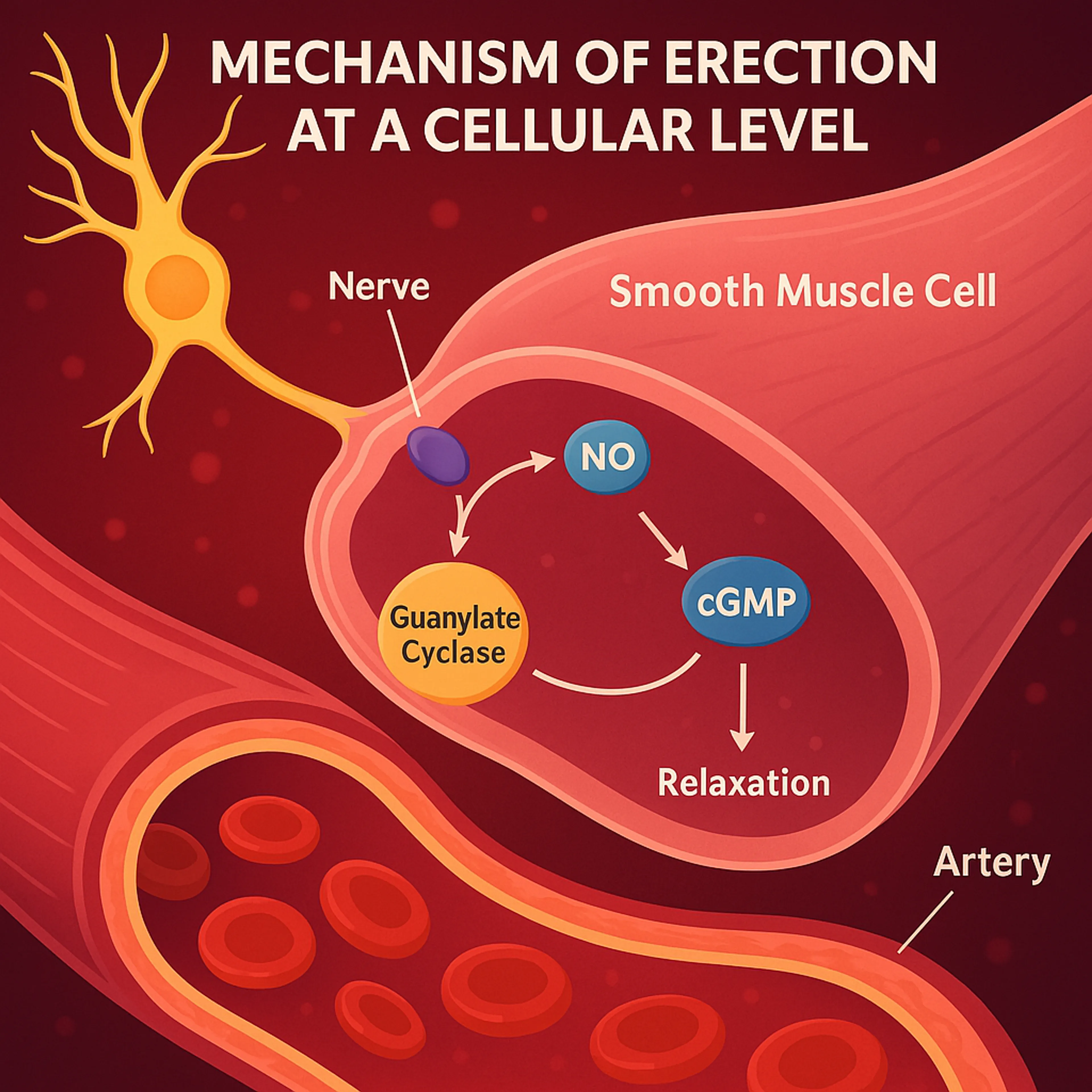
The Science of Erections: Your Body's Remarkable Mechanism
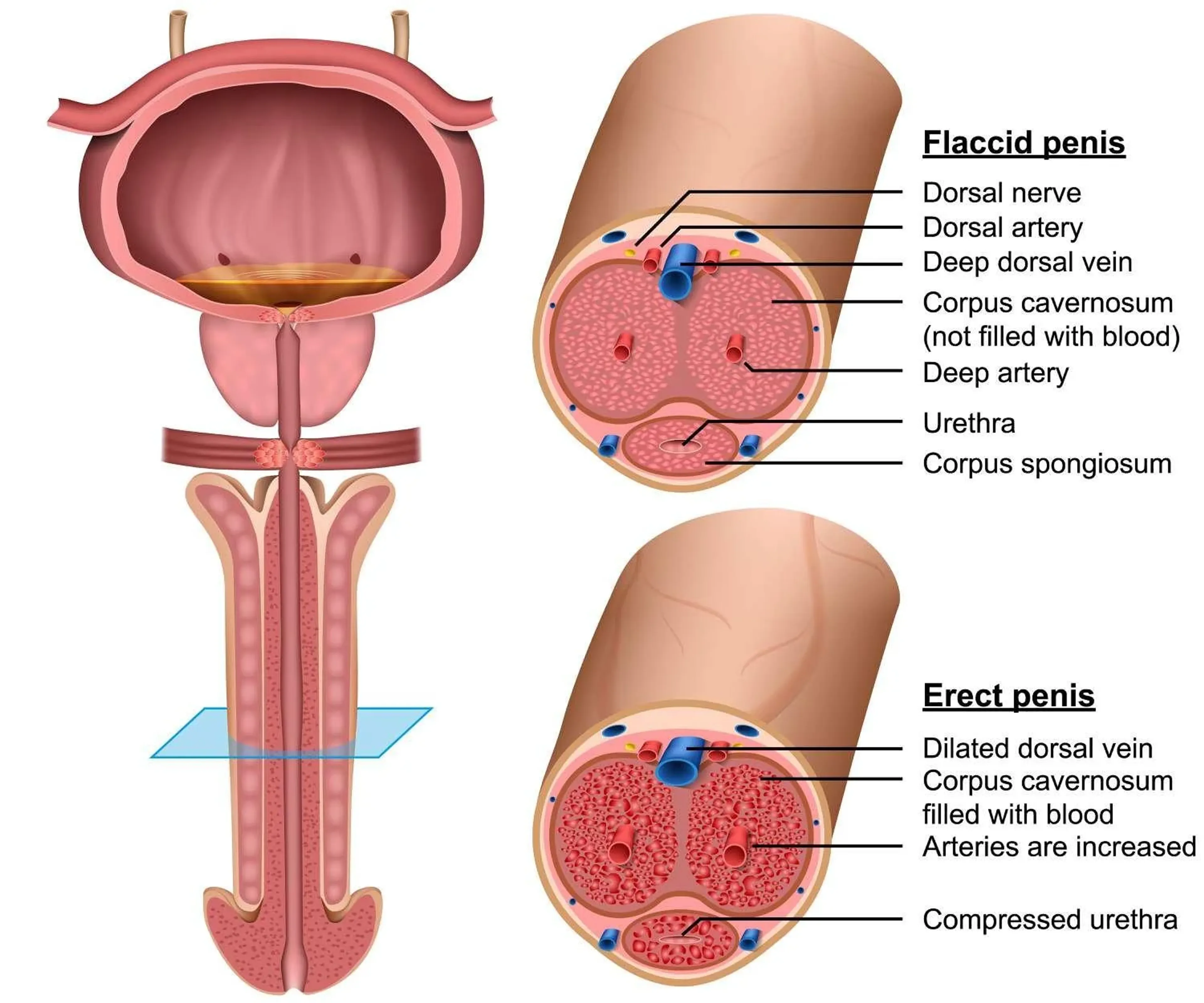
Achieving an erection is a sophisticated interplay involving the brain, nerves, hormones (like testosterone), and crucial vascular events within the penis. Triggered by arousal, nerve signals release Nitric Oxide (NO), leading to smooth muscle relaxation, increased blood flow into the erectile chambers (corpora cavernosa), and trapping of this blood (veno-occlusion) to create rigidity.
Physical Causes of ED: Understanding the Organic Factors
Often developing gradually, physical causes of erectile dysfunction commonly involve the body's hardware: issues with blood vessels (vascular disease - the most frequent cause, including arterial insufficiency or venous leak), nerve pathways (neurological disorders or injury), hormone levels (like low testosterone), side effects from various medications, or structural penile problems like Peyronie's disease.
Physical causes of Erectile Dysfunction
Psychological Causes of ED & Performance Anxiety: The Mind's Powerful Role
Summary: The brain plays a pivotal role in sexual function. Psychological erectile dysfunction arises when mental or emotional factors like stress, depression, relationship issues, or specific anxieties about sexual performance interfere with the signals needed for an erection, even if the physical 'plumbing' is healthy. Performance anxiety, a common trigger, creates a vicious cycle of worry and failure.
A metaphorical model explaining how stress and evolutionary survival mechanisms may cause performance anxiety and psychogenic erectile dysfunction.
While physical factors are often involved, especially as men age, the power of the mind in influencing sexual response cannot be overstated. Psychological erectile dysfunction (sometimes called psychogenic ED) occurs when mental or emotional processes disrupt the normal erectile cascade.
FAQ:Can ED be "only in my mind"?
Yes, absolutely. In cases of purely psychological ED, the physical structures—nerves, blood vessels, muscles—are capable of producing an erection. However, psychological factors intervene to prevent it. This typically happens in one of two main ways:
- Inhibition of Arousal Signals:Severe stress, depression, distraction, or lack of connection can prevent the brain from sending the necessary pro-erectile signals in the first place, regardless of physical stimuli.
- Activation of the Sympathetic Nervous System ('Fight-or-Flight'):This is the mechanism behind performance anxiety. Worrying about performance triggers an adrenaline surge, actively constricting penile blood vessels and tensing smooth muscles, making erection physically impossible at that moment.
Psychological ED is particularly common in younger men where underlying physical disease is less likely, but it can affect men of any age. Often, a pattern of good erections in low-pressure situations (e.g., waking erections, self-stimulation) but difficulty during attempted partner sex points strongly towards a significant psychological component.
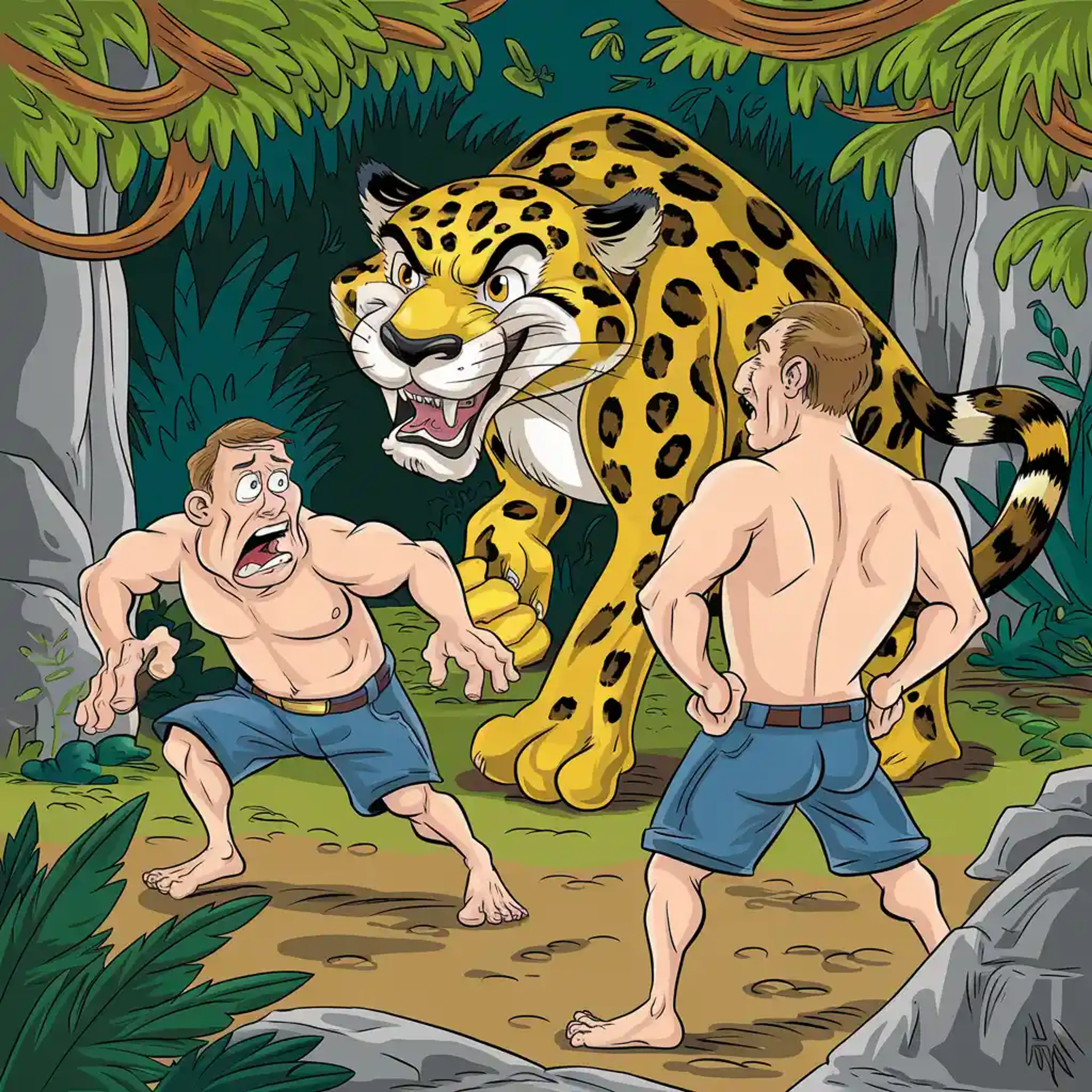
Understanding Performance Anxiety: The 'Jaguar in the Jungle' Analogy Explained
Performance anxiety ED is perhaps the most discussed psychological cause. The 'Jaguar in the Jungle' analogy helps illustrate the powerful physiological hijack that occurs:
- The "Threat": The brain perceives the sexual encounter not as pleasurable but as a performance test with a high risk of perceived failure (inability to get/keep an erection). This perception triggers an alarm signal.
- The Ancient Response: This alarm activates the sympathetic nervous system – the body's innate survival mechanism designed for immediate physical threats (like facing a predator).
- Adrenaline Surge: The adrenal glands release stress hormones, primarily adrenaline (epinephrine).
- Physiological Shift: Adrenaline causes widespread physiological changes to prepare for fight or flight: heart rate increases, breathing quickens, senses sharpen, and crucially, blood flow is redistributed.
- Blood Flow Diversion: Blood is shunted *away* from organs not essential for immediate survival (including the digestive system and the penis) and *towards* the large muscles of the limbs, heart, and brain.
- Anti-Erection State: Adrenaline directly causes constriction of the penile arteries and contraction of the smooth muscle within the corpora cavernosa. This actively prevents blood inflow and traps very little blood – the physiological opposite of what's needed for an erection.
- The Vicious Cycle: One episode of failure due to anxiety makes the man worry more about the next time. This increased worry makes the 'threat' seem larger, triggering an even stronger sympathetic response, making failure more likely, thus reinforcing the anxiety. This cycle can quickly become established and difficult to break without intervention.
Effectively, performance anxiety turns intimacy into a perceived survival situation, physiologically blocking the body's ability to respond sexually.
Myth Buster:"Porn caused my erectile dysfunction!"
The idea of "Porn-Induced Erectile Dysfunction" (PIED) is popular in online forums but lacks formal recognition as a distinct medical diagnosis in major classifications like DSM-5 or ICD-11. While there's no doubt excessive internet pornography consumption can correlate with sexual difficulties for *some* men, causality is complex and often debated. Potential contributing factors linked to heavy use might include:
- Unrealistic Expectations:Comparing real-life partners and encounters to the often artificial and high-stimulation scenarios in porn.
- Desensitisation:Requiring increasingly intense or novel stimuli for arousal, making normal intimacy seem less stimulating.
- Performance Anxiety:Feeling pressure to 'perform' like actors in porn.
- Associated Factors:Heavy porn use might coexist with underlying anxiety, depression, relationship issues, guilt, or low self-esteem, which are themselves established causes of ED.
It's rarely accurate to attribute ED solely to porn use without a thorough assessment exploring potential underlying physical causes (vascular, neurological, hormonal) and other psychological factors. Often, problematic porn use is a symptom or coping mechanism related to other issues, rather than the primary cause itself. A balanced approach involves evaluating all potential contributors.
Other Key Psychological Contributors to ED:
- Generalised Anxiety Disorder (GAD) & Other Anxiety States: Chronic worry, panic attacks, social anxiety – high baseline levels of anxiety can easily interfere with the relaxation needed for sexual response.
- Depression: Clinical depression is strongly linked to ED. Symptoms like low mood, loss of interest/pleasure (anhedonia), fatigue, feelings of worthlessness, and changes in sleep/appetite directly impact libido and erectile capacity. Furthermore, some antidepressant medications can also cause ED as a side effect (see Physical Causes).
- Chronic Stress: Ongoing high levels of stress from work, finances, family responsibilities, or life events elevate cortisol and adrenaline, suppressing the parasympathetic (relaxation) response needed for erection and potentially lowering testosterone over time.
- Relationship Conflict & Intimacy Issues: Lack of emotional connection, unresolved anger or resentment, poor communication, boredom, or fear of intimacy with a specific partner can profoundly inhibit sexual arousal and function, even if erections are possible in other contexts.
- Past Trauma or Negative Sexual Experiences: History of sexual abuse, assault, embarrassing early experiences, or upbringing with negative messages about sex can create deep-seated psychological blocks to healthy sexual function.
- Low Self-Esteem & Body Image Issues: Feeling unattractive, inadequate, or ashamed of one's body can inhibit sexual confidence and arousal.
- Sexual Orientation Conflicts or Guilt: Unresolved issues or guilt surrounding sexual identity or preferences can manifest as ED.
- Fear of Pregnancy or STIs: While less common as a primary cause, significant anxiety about consequences can sometimes interfere with performance.
The Interplay: Mixed ED is Common
It's critically important to reiterate that ED is often multifactorial. A man might start with mild physical ED due to developing vascular disease. This physical change then triggers performance anxiety, making the ED much worse than the physical component alone would suggest. Conversely, chronic stress might contribute to both psychological ED and worsen physical factors like high blood pressure over time. Effective management often requires addressing *both* the physical and psychological contributors simultaneously.
Is it psychological or physical?
This is one of the most important reframes:
"Psychological" doesn't mean "not real". It means the nervous system is interrupting the erection process—often through anxiety, stress, distraction, or learned fear of failure.
And "physical" doesn't mean "hopeless". It means we look at blood flow, nerves, hormones, medications, and penile tissue—and treat the part that's limiting you.
Clues that anxiety may be a major driver
Clues that physical factors need attention
Knowledge check
Which statement best describes your pattern?
This isn't a diagnosis—just a thinking tool.
ED treatment ladder (in 60 seconds)
Most erectile dysfunction treatment follows a sensible progression—but the key is matching treatment to the mechanism, not just trying things in order.
The typical pathway (when diagnosis is clear)
- Optimise risk factors: Sleep, alcohol, smoking cessation, weight management, cardiovascular fitness, medication review
- PDE5 inhibitors done properly: Correct dose, timing, stimulation, and realistic expectations (sildenafil, tadalafil, others)
- Psychosexual support: If performance anxiety, stress, or relationship dynamics are driving the pattern—sometimes alongside medical treatment
- Second-line options: Vacuum devices, injection therapy (when appropriate and with proper training)
- Surgical options: Penile implants for severe ED when other treatments fail
Important: Success is reliable function + satisfaction—not a porn script. We define outcomes based on what matters to you.
This ladder assumes we understand the mechanism. If we're guessing, or if first-line treatment fails, that's when assessment and sometimes objective testing becomes essential.
Read detailed treatment options below
Quick self-assessment (IIEF-5)
The International Index of Erectile Function (IIEF-5) is a brief, validated questionnaire used worldwide to quantify erectile dysfunction severity. It's not a diagnosis—it's a structured way to describe your pattern.
Important context before you score yourself: A score can change with stress, alcohol, relationship context, mood, and expectations. We use it to track change and structure the conversation—not to label you.
Complete the IIEF-5 (2 minutes)
Your score helps structure the conversation at your consultation—but it doesn't tell us why erectile dysfunction is happening. That's what assessment is for.
What IIEF-5 scores mean (and what they don't)
How I assess erectile dysfunction
There's a reason online "one-pill-fits-all" erectile dysfunction treatment approaches disappoint: without diagnosis, you can end up treating the wrong problem.
In my London practice, I see erectile dysfunction every week—and the pattern is rarely "one cause". The assessment clarifies what's driving your symptoms, so we can match treatment to mechanism.
Step 1: A focused, non-awkward history
- Onset (sudden vs gradual), variability, and what changes the outcome
- Libido, ejaculation, orgasm, penile pain/curvature, and any urinary symptoms
- I will ask you about night or early morning erections
- I will also ask you about erection when you do masturbation
- Cardiometabolic risk factors (blood pressure, diabetes, cholesterol, smoking, weight, sleep)
- Medications, alcohol, recreational drugs, stress, mood, and relationship context
Step 2: Examination
It involves the abdomen and genitals at least.
Usually brief: blood pressure, body habitus, genital examination, signs of penile plaque, and sometimes prostate assessment depending on symptoms.
Step 3: Targeted blood tests
Often includes lipids, glucose/HbA1c, and—when indicated—hormones such as testosterone (typically before 11am, with repeat testing and additional markers like SHBG, LH, FSH as appropriate if initial results are abnormal).
Most erectile dysfunction can be managed without imaging
A lot of ED improves once we get the basics right: addressing risk factors, optimising sleep and alcohol intake, correcting tablet use, and tackling performance pressure. We move to objective testing only when it will change decisions.
When testing helps (and when it doesn't)
First: the point of investigations is not to impress you with a test. It's to stop us guessing when the stakes are higher.
A penile Doppler ultrasound doesn't "grade your masculinity" and it doesn't diagnose relationship issues. It helps us decide whether the main driver looks vascular and/or structural, and whether treatments aimed at blood flow are likely to work.
A Doppler is not for everyone—but it is essential before certain treatments.
When objective testing commonly adds value
- You've tried first-line erectile dysfunction treatment properly and results are inconsistent or poor
- ED after pelvic/prostate surgery, radiotherapy, or significant pelvic trauma
- The picture is mixed and the "why" is unclear
- You're considering next-step treatments where
- cause matters
- You want objective answers rather than reassurance alone
When testing may not add much
- Clear, situational ED with strong performance anxiety features and otherwise reassuring clinical picture
- Early/mild erectile dysfunction that responds well to first-line treatment
- Situations where the result won't change your management choices
About penile Doppler ultrasound
Knowledge check
Which statement is most accurate?
Do I Need a Penile Doppler Ultrasound?
Penile Doppler Ultrasound is a very good test but for very few, selected cases. Most men with erectile dysfunction do not need imaging at the start. Tests like penile Doppler are used only when results change treatment decisions.
ED and testosterone: libido vs erection
Testosterone is often blamed for erectile dysfunction, but it helps to separate two things:
- Libido (desire): testosterone can influence this strongly in some men
- Erection mechanics: blood flow, nerve signalling, and penile tissue response are usually the limiting steps
Low testosterone can contribute to ED in some men—especially when libido is low—but it's not the automatic explanation. If hormones are part of the picture, we confirm it with properly timed blood tests (typically before 11am, with repeat testing if initial results are abnormal, plus additional markers like SHBG, LH, and FSH as appropriate) and interpret the results in clinical context.
When to check testosterone
ED and heart health
Erectile dysfunction isn't always a heart problem—but the penis is a blood-flow organ. Vascular issues can show up there earlier than they show up elsewhere.
If ED is new, persistent, and you also have cardiovascular risk factors (smoking, diabetes, high blood pressure, high cholesterol, excess weight, low activity, poor sleep), it's sensible to use this as a prompt to review overall cardiovascular health. That may involve your GP as well as specialist assessment.
Urgent medical help needed if you have:
- Chest pain on exertion or at rest
- Severe breathlessness
- Fainting or loss of consciousness
- Neurological symptoms (weakness, numbness, speech changes, visual changes)
If you're worried ED is a sign of something serious
Medications that can contribute to erectile dysfunction
Several common medications can affect erectile function. This doesn't mean they're wrong for you—it means we need to balance benefits and side effects, and sometimes adjust treatment.
Critical: Don't stop medications without medical advice. Some conditions require continuous treatment, and stopping suddenly can be dangerous.
Common medication categories that may contribute to ED:
- Antidepressants: Particularly SSRIs and SNRIs (e.g., sertraline, citalopram, venlafaxine)
- Antihypertensives: Some blood pressure tablets, particularly older beta-blockers and thiazide diuretics
- 5-alpha reductase inhibitors: Finasteride, dutasteride (used for prostate enlargement or hair loss)
- Opioid painkillers: Long-term use can affect hormone levels and sexual function
- Antipsychotics: Can affect dopamine and prolactin levels
- H2 antagonists: Cimetidine and similar medications for acid reflux (less common with newer PPIs)
If you suspect medication is contributing, discuss this with your prescribing doctor. There are often alternatives or additional treatments that can help manage erectile dysfunction while continuing necessary medication.
Many men worry that their medication is causing erectile dysfunction. While certain drugs can contribute, in many cases ED is linked to the health condition being treated, rather than the medication itself.
Treatment options (detailed)
There are several effective erectile dysfunction treatment options. The trick is matching the right tool to the right mechanism—and being honest about what we do and don't know.

Often first-line
- Lifestyle and risk-factor optimisation (sleep, alcohol, smoking cessation, weight management, cardiovascular fitness, medication review)
- Cardiovascular Health Focus: Since vascular disease is the most common cause, managing risk factors is key: controlling blood pressure, diabetes, and cholesterol levels; stopping smoking; maintaining a healthy weight; and regular aerobic exercise [Ref 5, 14].
- Dietary Changes: Emphasising a diet rich in fruits, vegetables, whole grains, fish, and nuts (like the Mediterranean diet) and low in red/processed meats, refined grains, and sugary drinks supports endothelial health and blood flow.
- Exercise: Regular moderate-to-vigorous aerobic exercise has been shown to improve erectile function, likely by improving blood flow, endothelial function, and reducing cardiovascular risk.
- Weight Loss: For overweight or obese men, losing weight can improve testosterone levels, insulin sensitivity, and vascular health.
- Smoking Cessation: Quitting smoking provides rapid and significant benefits to vascular health.
- Alcohol Moderation: Reducing excessive alcohol intake is important for nerve function and overall health.
- Stress Reduction & Sleep: Managing chronic stress and ensuring adequate sleep quality can positively impact hormonal balance and autonomic nervous system function.
- PDE5 inhibitors (e.g., sildenafil/Viagra, tadalafil/Cialis): effective for many men with erectile dysfunction, but not magic—dose, timing, stimulation, and expectations matter
Phosphodiesterase type 5 inhibitors (PDE5i) are the most commonly prescribed medical treatment for ED and have revolutionized management since their introduction. They are effective for many men, particularly those with mild to moderate ED, or ED related to psychogenic causes or mild vascular issues.
- Mechanism of Action: They block the PDE5 enzyme in the penis, preventing the breakdown of cGMP. This allows cGMP levels to build up in response to sexual stimulation and NO release, promoting smooth muscle relaxation, increased blood inflow, and firmer, longer-lasting erections. They require sexual stimulation to be effective.
- Available Options in the UK:
- Sildenafil (Viagra, Viagra Connect): The first PDE5i. Onset typically 30-60 minutes, duration about 4-5 hours. Absorption can be delayed by high-fat meals. Viagra Connect is available OTC after pharmacist assessment.
- Tadalafil (Cialis, Cialis Daily): Characterised by a much longer duration of action (up to 36 hours), offering greater spontaneity ("the weekend pill"). Absorption is not significantly affected by food. Available as 'on-demand' doses (10mg, 20mg) or a low daily dose (2.5mg, 5mg) for continuous effect.
- Vardenafil (Levitra): Similar profile to sildenafil (onset ~30 mins, duration 4-5 hours). Some men may respond better to vardenafil if sildenafil is ineffective. Food effect similar to sildenafil.
- Avanafil (Spedra): A newer generation PDE5i with potentially faster onset (15-30 minutes for some) and similar duration to sildenafil/vardenafil. May have slightly higher selectivity for PDE5, potentially reducing some side effects.
- Efficacy: Success rates are generally 60-80%, depending on the cause and severity of ED. Less effective in severe vascular disease, significant nerve damage (e.g., post-prostatectomy), or severe diabetes.
- Clinical Pearls & Patient Guidance:
- Multiple Trials Needed: Don't give up after one try. It often takes 4-8 attempts with adequate stimulation to determine if a specific PDE5i at an optimal dose works for you.
- Timing is Key: Take the medication appropriately before anticipated sexual activity (allowing for onset time).
- Stimulation is Required: These drugs enhance a natural response; they don't create desire or erections without arousal.
- Side Effects: Common side effects are usually mild and transient, including headache, facial flushing, nasal congestion, indigestion, and occasionally visual disturbances (blue tinge - sildenafil) or back/muscle pain (tadalafil).
- Safety and Contraindications: The primary contraindication is concurrent use of nitrates. Caution is needed with certain heart conditions and with alpha-blocker medications for BPH (potential for low blood pressure). A prescription requires a prior medical assessment.
- Psychosexual support when anxiety, stress, shame, avoidance, or relationship dynamics are central (sometimes alongside medical treatment)
How to avoid 'false failures' with tablets
When first-line isn't enough
- Vacuum erection devices
- (mechanical option; some couples find them helpful, some don't—worth trying before more invasive options)
- Intracavernosal injection therapy
- (highly effective in selected men; requires safe teaching and clear discussion of risks including priapism)
- Penile implants
- (a reliable surgical option for severe erectile dysfunction when other treatments fail; involves surgery and irreversible change)
About 'regenerative' or device-led treatments
Common side effects include headache, flushing, indigestion, and nasal congestion. They are not suitable with certain heart medications (especially nitrates used for angina). We check your medical history and current medications before prescribing erectile dysfunction treatment.
Can cause pain, bruising, and rarely a prolonged erection (priapism), which needs urgent treatment. Proper training and dose titration reduce risks significantly. Not suitable for all men—requires assessment and supervised initial use.
Surgery carries risks including infection, mechanical failure over time, and revision surgery. Modern devices have good reliability, but this is an irreversible change that requires careful decision-making. We only recommend this when other erectile dysfunction treatments have genuinely failed.
What to do now
Most efficient pathway
- Clinician-led erectile dysfunction assessment (history + targeted blood tests)
- Trial first-line treatment properly (correct dose, timing, stimulation, realistic expectations)
- If unclear, not working, or considering next steps → objective data when it changes decisions
If you want the most efficient path, keep these two questions in mind:
- What's the likely driver (vascular, hormonal, neurological, psychological/relational, medication-related, structural—or a mix)?
- Will objective data change what we do next?
Next steps
Choose your starting point
Start with assessment
If you want a clinician-led plan first, we'll begin with a confidential consultation and targeted tests, then decide what adds value.
If anxiety is central
That doesn't mean "it's not real". It means the most effective plan may combine medical support with targeted psychosexual strategies—without shame.
Understanding objective testing
If decisions depend on blood flow—or you're stuck—read about when Doppler clarifies the pathway.
Your next steps
Erectile dysfunction is treatable. But the best outcomes come from matching the treatment to the mechanism. If you're at the point where "trying another pill" isn't good enough, structured assessment can be the difference between guessing and choosing well.
Book your erectile dysfunction assessment
Further readings and references
Sexual Advice Association (UK): Comprehensive factsheets on ED, injections, and vacuum pumps.
NHS - Erectile Dysfunction: A clear overview of symptoms and NHS pathways.
British Association of Urological Surgeons (BAUS): Patient leaflets on penile implants and Peyronie's disease.
Diabetes UK: Managing sexual problems when living with diabetes.
The assessment and treatment pathways on this page are based on the following international clinical standards:
- EAU Guidelines on Sexual and Reproductive Health: The European Association of Urology (EAU) updates these annually. They provide the gold standard for ED diagnosis and the "Treatment Ladder."
- Salonia A, et al. EAU Guidelines on Sexual and Reproductive Health. 2024.
- BSSM Guidelines on Adult ED: The British Society for Sexual Medicine (BSSM) provides specific UK-focused clinical protocols.
- Hackett G, et al. British Society for Sexual Medicine Guidelines on the Management of Erectile Dysfunction in Men. 2018/Updated.
- The Princeton III Consensus: This provides the clinical framework for the evaluation of cardiac risk in men with ED.
- Nehra A, et al. The Princeton III Consensus Conference Management of Erectile Dysfunction and Cardiovascular Disease. Mayo Clin Proc. 2012.
- IIEF-5 Validation: The original study validating the International Index of Erectile Function.
- Rosen RC, et al. The International Index of Erectile Function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997.
- Vascular Mechanisms & Doppler: Research on the efficacy of Penile Doppler Ultrasound in diagnosing veno-occlusive dysfunction.
- Sikka SC, et al. Standardization of Vascular Assessment of Erectile Dysfunction. Journal of Sexual Medicine. 2018.
Medical disclaimer: This information is for general education only and cannot replace personalised medical advice. If you're concerned about erectile dysfunction or related symptoms, please speak to a GP or specialist urologist.