Worried about a bend or change in your penis? You're not alone — and there are real options.
Peyronie's disease affects around 1 in 10 men. It's not cancer, it's not your fault, and it's very treatable. Mr Ollandini offers expert, confidential assessment and personalised care in London.
If you have noticed a new curve, bend, or pain in your penis during an erection, it is completely natural to feel worried — and perhaps embarrassed to talk about it. Many men wait months or even years before seeking help. Often this is because they do not know where to turn, or they assume nothing can be done. The truth is, Peyronie's disease is one of the most common conditions seen in men's health clinics. It is well understood, and there are effective treatments available. You do not have to manage this alone. Seeking advice early almost always leads to better outcomes.
Key Points at a Glance
- Peyronie's is common: It affects around 1 in 10 men — you are far from alone.
- It is not cancer: Peyronie's disease is a benign (non-cancerous) condition and does not increase your risk of cancer.
- It is not your fault: Peyronie's is a biological wound-healing disorder — it is not caused by anything you did wrong.
- Treatment options exist: Both non-surgical (traction therapy, injections, shockwave) and surgical options are available depending on your situation.
- Two distinct phases: The acute (active) phase involves ongoing scarring and pain. The stable phase means the plaque has settled. Treatment strategy differs between the two.
- Early assessment matters: Getting help during the acute phase opens up more treatment options and may stop the condition from getting worse.
On This Page
Why is my penis curved or painful when erect?
A new curve, bend, or pain in the penis during an erection can be alarming. This is especially true if it appears suddenly or gets worse over time.
In many men, this change is caused by Peyronie’s disease, a condition where scar tissue (fibrosis) forms inside the tunica albuginea (the strong, stretchy layer that lets the penis expand during an erection).
Unlike a natural variation in shape, curvature caused by Peyronie's disease is often:
- Acquired, not lifelong
- Associated with pain, especially in the early phase
- Getting worse over months, rather than staying the same
Importantly, this is not a disease of hygiene, sexual behaviour, or "doing something wrong". It is a biological wound-healing disorder, often triggered by minor penile trauma that the person may not even remember.
The first question most men ask is:
"Why is my penis bent or painful when erect?"
In clinical terms, the answer is usually clear: because Peyronie’s disease is present.
A deeper question often follows:
"Why did I develop Peyronie's disease?"
This second question is understandable. But in medical practice, it is very often impossible to answer with certainty, and in most cases does not change how the condition is managed.
Peyronie's disease is not caused by one single, clear event in most men. Instead, it seems to involve a complex mix of tissue biology, healing responses, and individual susceptibility. Minor or repeated stress to the penis may play a role in some cases. But many men develop Peyronie's disease with no clear history of injury or trauma.
For this reason, trying to find a single "cause" is often not clinically useful. What matters far more is:
- Whether the disease is active or stable
- How much pain, curvature, or shortening is present
- Whether erectile function is affected
- How the condition is affecting quality of life
These factors — not the presumed origin of the disease — are what guide treatment decisions and outcomes.
Feeling Concerned About a Bend or Change?
It is understandable to feel worried if you notice a bend, curve, lump, or pain in your penis. It is a personal issue, and many men hesitate to seek help because of uncertainty or embarrassment. If you have been searching for "bent penis" or penile curvature, a common cause is Peyronie's disease (sometimes called Peyronie disease). You are not alone, and expert help is available.

It's completely understandable to feel anxious or distressed when you observe structural changes or discomfort in your penis. It’s a deeply personal experience. Some men I see in my clinic seek help straight away, while others, perhaps due to embarrassment or simply not knowing where to turn, wait months or even years. If terms like "lump in penis," "painful erection," "bent willy," or noticing a change in shape resonates with your experience, understanding Peyronie's disease is the crucial first step towards finding solutions and exploring available treatment. Remember, seeking advice sooner rather than later often leads to better outcomes and more treatment options.
Ready to understand what is happening with your penis?
What is Peyronie's Disease? The Basics
Key Insight: Peyronie's disease involves fibrous scar tissue (plaque) forming inside the penis. This happens within a layer called the tunica albuginea (the strong outer sheath of the penis). This inelastic plaque — essentially scar tissue — disrupts how the penis works during an erection. It causes bending (penile curvature), pain, and sometimes difficulty with sex or erectile dysfunction (ED). It is more common than many people realise, affecting up to 1 in 10 men, particularly as they get older. While it is not usually "cured" without surgery, this disease is manageable with effective treatments that focus on improving function and quality of life.
Peyronie’s disease is not dangerous or life-threatening. However, it can significantly affect sexual function, confidence, and quality of life, which is why proper assessment and management are important.
In some men, Peyronie’s disease progresses over months before stabilising. In others, changes remain mild. Progression depends on the disease phase and individual factors.
Peyronie’s disease can be associated with erectile dysfunction, particularly when curvature, pain, or tissue stiffness interfere with normal erection mechanics.
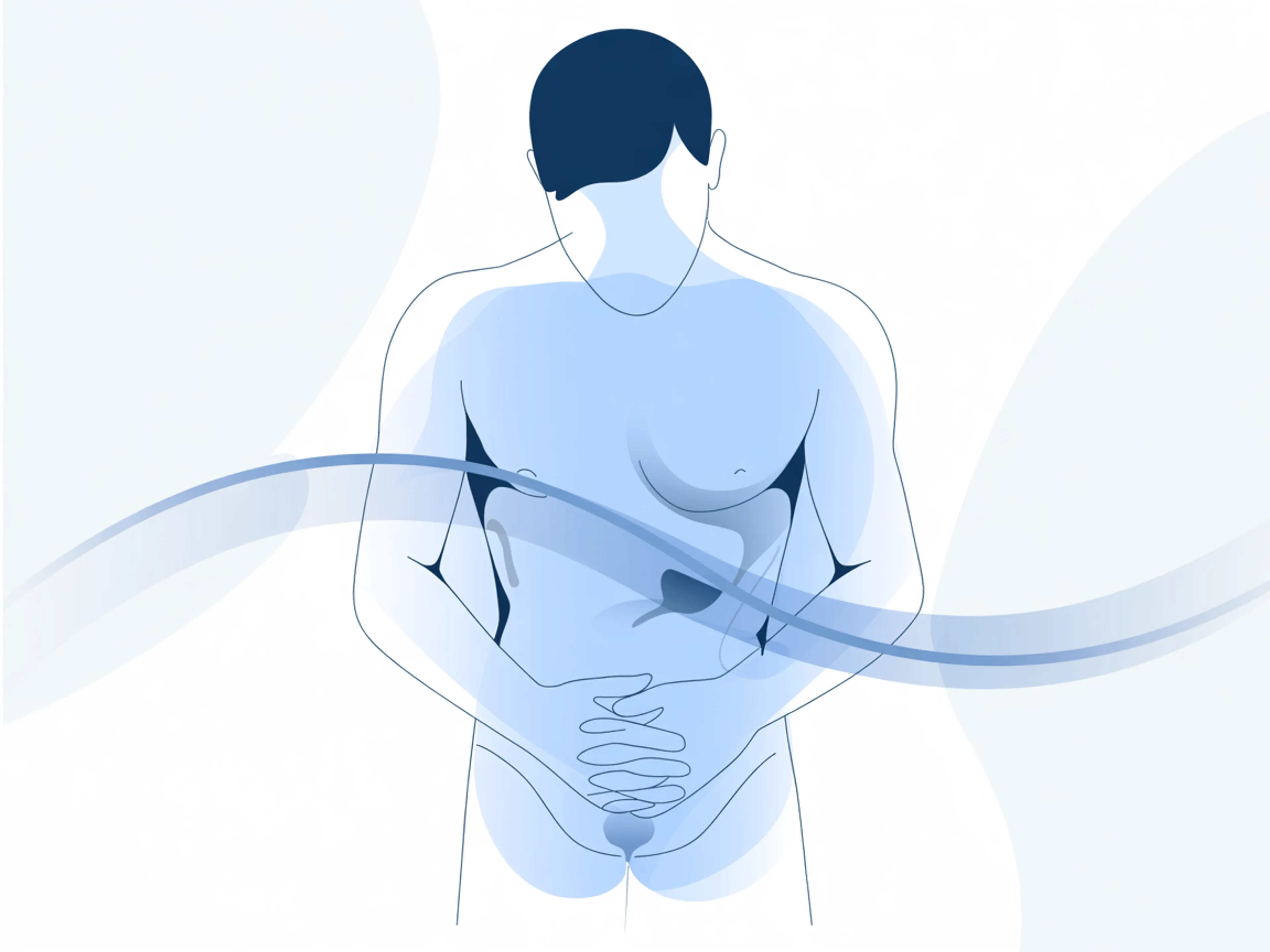
As a Consultant Urological Surgeon specialising in men's health and andrology, I want to offer clear, honest guidance. Peyronies disease fundamentally involves the development of fibrous plaque within the tunica albuginea – the specialised fibrous sheath surrounding the erectile chambers (corpora cavernosa) of the penis. This layer is crucial for erections; its relative inelasticity helps contain the increased blood pressure, creating penile rigidity. In Peyronie's disease, the inelastic plaque disrupts this normal physiological process, preventing symmetrical expansion and causing the characteristic bent penis that many find distressing.
It's far more common than most men realise, yet frequently under-diagnosed, often due to embarrassment or a lack of awareness about available Peyronie's disease treatment options. My focus isn't necessarily on a "Peyronie's disease cure" that eliminates every trace of the plaque, but on effectively managing your symptoms – the pain, the curvature, the ED – to significantly improve function and quality of life. Early intervention regarding treatment is key, as it offers the best chance of success and potentially minimising the impact of the condition.
Take the first step towards understanding and managing this disease.
Peyronie's Disease: A Closer Look
Understanding Peyronie's: This condition centres on the tunica albuginea, where plaque (fibrous scar tissue) forms. It is often triggered by minor penile trauma — small injuries that lead to abnormal scarring. Genetics and blood vessel health may also play a role. The disease usually goes through two stages: an early Acute (Active) Phase (often painful, with a changing curve) and a later Stable (Chronic) Phase (pain usually gone, curve fixed). Key risk factors include age, genetics (such as Dupuytren's contracture), cardiovascular issues (diabetes, high blood pressure, smoking), and possible penile injury.
Understanding the Cause: Tunica Albuginea, Plaque, and Mechanisms
The tunica albuginea is the key structure involved. Plaque formation – essentially abnormal collagen deposition resulting in fibrous scar tissue – within this layer disrupts its normal function during erection. Instead of expanding evenly, the scarred area tethers the tissue, causing the bend, penile nodules, narrowing ('hourglass deformity'), or even penile shortening. Recent research confirms Peyronie's affects roughly 5-10% of men globally, increasing significantly after age 50, though I suspect the true figure might be higher given how many men delay seeking help.
What causes Peyronie's disease?
The development involves a complex cascade of pathophysiological events. Key mechanisms identified by scientific research include:
- Trauma-Induced Inflammation: The leading theory suggests microscopic injuries or repetitive micro-trauma during sexual activity trigger an abnormal wound healing response in susceptible individuals, leading to excess scar tissue.
- Myofibroblast Proliferation: Specialised cells multiply excessively, producing excessive scar tissue components.
- Dysregulated Collagen Production: Abnormal deposition of Type I and III collagen creates the dense, inelastic plaque, which can sometimes become calcified (hardened).
- Autoimmune Factors: Some evidence suggests the immune system might mistakenly contribute to the inflammation and plaque formation.
Triggers and Risk Factors
While the exact trigger often remains unclear, several factors contribute:
- Penile Trauma: Both acute injuries and repetitive microtrauma to the penis.
- Genetic Predisposition: A strong link exists with other fibrotic conditions like Dupuytren's contracture (hand) and Ledderhose disease (foot), suggesting a genetic component.
- Cardiovascular Risk Factors: Hypertension, hypercholesterolemia, diabetes, and smoking significantly increase risk, likely by affecting blood vessel health and wound healing. Can diabetes cause Peyronie's disease? While not a direct cause, it's a major risk factor.
- Injection-Related Factors: Repeated use of intracavernosal injections for ED is occasionally implicated.
- Can circumcision cause Peyronie's disease? There is no established link.
Often, it's likely a combination of these factors at play in the development of this disease.
The Two Phases: Acute vs. Stable - Why Timing Matters
Recognising the disease phase is crucial for determining the appropriate Peyronie's disease treatment strategy:
- Acute (Active) Phase:
- Initial inflammatory period (lasts ~6-18 months) with active plaque formation. This is often called the acute phase.
- Penile pain during erections is common (present in 35-45% of patients).
- Penile curvature may progressively worsen or change during this time. Penile shortening can also occur.
- This phase is often the optimal timing for considering non-surgical treatment options aimed at minimising progression and managing pain (e.g., penile traction therapy, oral medications, potentially Li-ESWT for pain).
- Stable (Chronic) Phase:
- Follows the active phase once inflammation subsides and plaque formation ceases.
- Plaque typically stabilises without further progression; the fibrous scar tissue matures.
- Penile pain usually resolves spontaneously by this stage.
- The established penile curvature becomes fixed.
- Surgical treatment interventions to correct curvature are generally considered only once this phase is reached.
Is Peyronie's disease permanent?
The plaque itself often persists, but the symptoms are manageable, and the curvature can frequently be corrected surgically once stable.
Can Peyronie's disease heal itself or go away?
While pain often subsides, significant spontaneous improvement in curvature is rare (estimated around 10-15%). Most men find their curvature either stabilises or worsens without specific treatment.
Concerned about your symptoms or which phase you might be in? Let's talk.
Key Symptoms of Peyronie's Disease
Recognising the Signs: Men with Peyronie's disease usually notice one or more key symptoms. These include a clear penile curvature or bend during erection, painful erections (especially early on), a hard lump or plaque (fibrous scar tissue) under the skin (penile nodules), new or worsening difficulty getting or keeping an erection (erectile dysfunction affecting sexual function), and sometimes a noticeable reduction in penile length or girth. These symptoms can appear suddenly or build up gradually.
Peyronie's typically manifests with a combination of these symptoms, known as the clinical triad plus associated features:
- Penile Curvature / Deformity: The hallmark symptom. The bend can be upwards, downwards, or sideways (why does it curve to the left? just depends on where the plaque forms). Some men develop indentations, narrowing ('hourglass' shape), or a generally odd shaped penis. Viewing bent penis pictures or curved penis pictures online may prompt men to recognise their own condition.
- Penile Pain: Particularly pain during erection or intercourse, common in the early (acute) phase. Often described as an ache or soreness within the penile shaft. Thankfully, this penile pain usually resolves spontaneously as the condition stabilises.
- Erectile Dysfunction (ED): Difficulty achieving or maintaining an erection sufficient for sexual activity affects a large proportion of men with Peyronie's disease (up to 80% in some studies). This dysfunction penile can stem from the pain, the mechanical difficulty caused by the curve, impaired blood flow (venous leak), associated erectile dysfunction nerve damage symptoms in some, or the psychological impact. ED significantly impacts sexual function.
- Palpable Plaque: Many men (or their partners) can feel a distinct hard lump, nodule, or thickened area under the skin – this is the Peyronie's plaque itself, composed of fibrous scar tissue. While finding a lump can be worrying, in this context, it's characteristic of the condition.
- Penile Shortening: Unfortunately, contraction of the plaque can pull on surrounding tissues, leading to a gradual loss of penile length, which can be very distressing. Some men also notice a loss of girth.
The severity and combination of symptoms vary greatly. For some, the visual appearance of the bent penis is the primary concern; for others, it's the functional limitation or pain associated with this disease.
Diagnosing Peyronie's: Consultation and Assessment
Getting Clarity: Finding out if you have Peyronie's disease involves a careful process. It starts with talking about your symptoms and medical history. A physical examination helps find the characteristic plaque (fibrous scar tissue). It's important to measure any curvature accurately. The best way to do this is usually through erection photographs that you take privately at home (following specific guidelines, ideally repeated after 3 months to check stability). Alternatively, an in-clinic injection (ICI test) or a specialised Penile Doppler Ultrasound can produce an erection for precise measurement and analysis of penile blood flow. This is especially useful if erectile dysfunction is also present.

An accurate diagnosis is the foundation for effective treatment planning for this disease.
- Your Consultation: We'll have a detailed discussion about when symptoms started, what bothers you most (curve, pain, ED, shortening, lump), whether things are changing, the impact on your sex life and confidence, and any relevant medical history or risk factors (like diabetes, previous trauma, Dupuytren's). Understanding each symptom is crucial.
- Physical Examination: I will perform a careful examination of your penis in its flaccid state. Feeling for the characteristic palpable plaque – its location, size, texture – is key. While finding a lump can cause anxiety, in the context of Peyronie's symptoms, it's rarely sinister.
- Objective Curvature Assessment: Your description is helpful, but objective measurement is essential, especially for planning potential surgical treatment and assessing stability.
- Self-Photography (Preferred Method): Taking clear photographs of your fully erect penis from specific angles (top-down, side-on, front-on) at home is usually the best initial approach. Comparing photos taken at least three months apart is the gold standard for determining if the disease has reached the stable phase – a critical factor before considering surgery. (See detailed instructions in the How to Take Photos Section).
- In-Clinic Intracavernosal Injection (ICI) Test: If self-photography isn't possible or clear, we can induce an erection medically in the clinic using a small injection (e.g., prostaglandin E1). This allows me to directly measure the curvature degree with a goniometer and assess rigidity. Examination under Pharmacologically induced erection is usually required at least once to confirm the photographic findings before confirming the decision to go ahead with surgery.
- Penile Doppler Ultrasound: This advanced imaging is particularly valuable, especially if erectile dysfunction is a concern. Using sound waves during an induced erection, it can: clearly visualise the plaque(s) (size, location, calcification), provide precise curvature measurements, and critically, assess penile blood flow dynamics (arterial inflow and venous outflow/leak) to help diagnose the cause of ED. This helps evaluate the overall health of the penile tissue.
- Penile Doppler Ultrasound: This advanced imaging is particularly valuable, especially if erectile dysfunction is a concern. Using sound waves during an induced erection, it can: clearly visualise the plaque(s) (size, location, calcification), provide precise curvature measurements, and critically, assess penile blood flow dynamics (arterial inflow and venous outflow/leak) to help diagnose the cause of ED. This helps evaluate the overall health of the penile tissue.
Many men hope Peyronie's disease will "go away on its own"—while pain often does, significant curvature improvement is rare. Starting the diagnostic process early allows for timely intervention, potentially preventing worsening and reducing the need for later, more complex treatment.
Ready for an accurate assessment?
Ready to get a proper assessment?
A precise diagnosis is the foundation of effective treatment. Mr Ollandini offers expert Peyronie's assessment in London — including Penile Doppler Ultrasound and objective curvature measurement.
How to Take Erection Photographs: Safely and Effectively
Your Role in Diagnosis: Providing clear photographs of your erection is a standard and very useful part of the Peyronie's disease assessment. It allows for precise measurement of the curve and helps show whether the condition has stabilised — essential information for planning the right treatment. Remember to take images of a full erection from the top, side, and front. Ideally, repeat this after 3 months, keeping conditions the same. Privacy is very important: please never email these photos. Use the secure Carebit patient portal (link provided to patients) for uploading.
Erection photography might feel awkward, but it's an invaluable and standard diagnostic tool for Peyronie's disease. Comparing two sets taken ≥3 months apart is the most reliable way to see if the curvature is stable, guiding treatment decisions, particularly regarding surgery.
- Why Take Photos? To objectively measure the degree and direction of curvature, identify other deformities (narrowing), and assess stability over time.
- When? Take the first set as soon as possible after noticing changes. Take the second set ≥3 months later, replicating conditions (rigidity, angle, lighting) as closely as possible.
- How to Take Medically Useful Photos:
- Achieve a Full Erection: Must be maximum rigidity, similar to intercourse. Partial erection masks the true curve.
- Capture Three Clear Angles: Use timer or trusted partner. Get shots from: Top-down (bird’s eye), Side-on (lateral - showing curve best), and Front-on (anterior). Ensure the entire penile shaft is clearly visible in each.
- Use Good, Consistent Lighting: Natural light preferable. Avoid flash/shadows. Use a plain, neutral background.
- Frame Clearly: Show only the erect penis against the background. No hands, clothing, or distracting objects.
- Label or Date Images: Helps track timing (e.g., filename "PD_Photos_March_2025.jpg" or note in upload message).
- Uploading Securely - The ONLY Way: DO NOT use personal email - it's insecure. Use the encrypted, GDPR-compliant [Your Patient Portal Name, e.g., Carebit] patient portal provided to my patients. This ensures your images are stored securely within your confidential medical record, accessible only by me and authorised clinical staff. Contact my secretary if you need portal assistance. Contact Details.
- What Happens After Review? Assessing the photos allows us to determine stability, choose appropriate non-surgical or surgical options confidently, and monitor progress or treatment results.
- Respect & Clinical Purpose: I understand the sensitivity. Your images are treated with utmost respect and confidentiality, used solely for clinical assessment and planning your best care pathway. You're playing a key role in your diagnosis for this disease.
Need help or ready to upload securely?
Peyronie's Disease Treatment Options: Your Personalised Plan
Finding the Right Path: While the fibrous scar tissue (plaque) in Peyronie's disease often stays without surgery, the aim of treatment is to manage its effects: pain, erectile dysfunction (ED), and the penile curve. The best approach depends on your symptoms, personal goals, and whether the disease is currently active or stable. Pain usually gets better over time but can be managed well. ED linked to Peyronie's has several treatment options, from medicines to devices or implants. Correcting the curve involves non-surgical methods like penile traction therapy or injections (Xiapex®, when suitable and available), often used in the acute phase or for less severe stable curves. Surgical treatment procedures, such as straightening techniques or penile implants, are usually kept for the stable phase when the curve significantly affects sexual function.
A fundamental principle is that while we won't be usually able to eliminate the plaque itself (either surgically and non-surgically), we can significantly improve its functional consequences. The goal is realistic: better function, less distress, improved quality of life. Not everyone needs active treatment if symptoms are mild and non-bothersome. For those significantly affected by this disease, targeted therapies and treatment options offer real hope.
Managing Peyronie's-Related Pain (Primarily Acute Phase)
Pain during erection is common initially (in the acute phase) but usually resolves within 6-18 months as the condition stabilises. While waiting, relief strategies include:
- Simple analgesics (paracetamol) and anti-inflammatories (NSAIDs like ibuprofen).
- Oral medications like Potassium para-aminobenzoate (Potaba), Vitamin E, CoQ10 have limited/mixed evidence but are sometimes discussed.
- Low-Intensity Extracorporeal Shockwave Therapy (Li-ESWT): Good evidence supports its use primarily for reducing Peyronie's-related pain during the active phase. I offer this non-invasive treatment for appropriate patients focused on pain relief.
Treating Erectile Dysfunction (ED) in Peyronie's
Erectile dysfunction is common and requires a systematic approach, tailored to you:
- Lifestyle & Risk Factor Management: Addressing underlying issues like diabetes, high blood pressure, cholesterol, and stopping smoking is crucial for vascular health.
- Oral Medications (PDE5 Inhibitors): First-line therapy often includes sildenafil (Viagra), tadalafil (Cialis), vardenafil (Levitra), or avanafil (Spedra). Effective if underlying blood flow isn't severely compromised. Daily low-dose tadalafil might also have anti-fibrotic benefits in the active phase.
- Intracavernosal Injections (ICI): If pills fail, injecting medication (e.g., alprostadil - Caverject, Viridal; or combination - Invicorp) directly into the penis reliably produces erections.
- Vacuum Erection Devices (VEDs): Creates an erection mechanically using suction and a constriction ring. Also beneficial for penile rehabilitation, tissue oxygenation, and potentially preserving length alongside other therapies. How to use vacuum pump for Peyronie's disease? Requires specific instruction for optimal benefit.
- Li-ESWT: Some studies suggest it might also improve blood flow and aid erectile function, potentially used adjunctively.
- Penile Prosthesis (Implant) Surgery: A type of surgical treatment offering a definitive solution when Peyronie's coexists with severe, treatment-resistant ED. A penile implant addresses both issues simultaneously.
Correcting Penile Curvature: Non-Surgical Options
These aim to reduce curvature and minimise length loss, primarily used in the acute phase or for milder stable curves, or for those wishing to avoid surgery. Commitment is key:
- Penile Traction Therapy (PTT): Mechanical devices (e.g., RestoreX®, Andropenis®, PeniMaster® Pro) apply controlled, sustained stretching. Clinical studies show consistent daily use (often 3-8 hours/day for 3-6+ months) can achieve 10-30%+ curvature reduction and help preserve/regain length. Compliance is essential. Many of my patients have avoided surgery through dedicated use of penile traction therapy.
- Intraplaque Injections (Collagenase Clostridium Histolyticum - Xiapex®): The only approved drug treatment (US FDA approval as Xiaflex®). An enzyme injected into the plaque (fibrous scar tissue) breaks down collagen. Trials show ~34% average curve reduction vs placebo. Best for moderate dorsal curves (30-90°) with good ED. Involves multiple injection cycles plus specific penile modelling/stretching. Often combined with PTT. UK availability (as Xiapex®) has been limited due to cost/licensing. Requires administration by a trained specialist due to potential side effects (bruising, rare rupture).
- VEDs: Complementary role, potentially aiding tissue remodelling alongside traction.
Assessing Stability Before Surgery Remains Paramount
Surgery is generally reserved for the stable phase (no pain, curvature stable for ≥3-6 months, confirmed by photos). Operating earlier risks unpredictable results and recurrence.
Surgical Treatments for Peyronie's Disease (Stable Phase Only)
Considered when stable curvature significantly hinders intercourse or causes major distress, and non-surgical methods are insufficient/unwanted. Thorough pre-operative assessment of erectile function is critical. These surgical treatment options include:
- Penile Straightening Procedures (Corporoplasty - Requires GOOD Pre-op Erections):
- Tunical Shortening (e.g., Nesbit Procedure, Plication, Yachia): Shortens the convex side opposite the plaque. High straightening success rate (~85-95%), very low risk of worsening ED. Main drawback: inevitable penile shortening (approx. 1cm per 15° corrected). Best for moderate curves (<60-70°) in men with good initial length accepting this trade-off. The Nesbit's procedure is a well-established example of this treatment.
- Tunical Lengthening (Plaque Incision/Excision & Grafting): Aims to preserve length by cutting the plaque and filling the gap with graft material. Better for severe (>60-70°) or complex curves where length is a major concern. Main drawback: significantly higher risk of new or worsened post-op ED (15-25%+). In consultation, I tend to explain the advantage of incision plus grafting (also called the Lou Procedure) especially dedicated to those person with a penis affected by a such severe bending that represents a full barrier to any sexual intercourse.
- Penile Prosthesis (Implant) Implantation with Straightening Manoeuvres (for Concomitant ED):
Truth to be told, a straightening procedure will not improve erectile function; if ED and penile deviation co-exist, the straightening may be not the correct step in order to effectively restore sexual capacity. That's why, before considering surgery to correct the deviation, I need to verify that erections are good, either naturally or with medical treatment.
Penile implant insertion (malleable or inflatable) is the gold standard when significant Peyronie's and treatment-resistant ED coexist.
- Penile Prosthesis (Implant) Implantation with Straightening Manoeuvres (for Concomitant ED):
- Surgically replaces damaged erectile tissue with cylinders (a penile implant), restoring reliable rigidity.
- Allows simultaneous straightening via manual modelling or other techniques.
- High patient satisfaction. Penile implant surgery offers a combined solution.
My Patient-Centred Approach to Treatment
My philosophy is individualised, evidence-based, and built on shared decision-making. We focus on managing the functional impact – pain, ED, curvature. For curvature, we start conservatively where appropriate (traction, VEDs). If surgical treatment is needed (only when stable), meticulous evaluation of erections, curve severity, length, and your goals dictates the best approach (shortening vs lengthening vs implant). I ensure you fully understand the risks, benefits, and realistic outcomes of each treatment option. Success requires patience, realistic expectations, and collaboration.
What usually determines treatment choice
Treatment decisions in Peyronie's disease are not based on curvature alone. They usually depend on:
- Disease phase (active vs stable)
- Degree and direction of curvature
- Presence of pain
- Impact on sexual function
- Individual priorities and expectations
For this reason, management is highly individualised and often changes over time.
Ready to discuss a treatment plan tailored to you?
Want a personalised treatment plan?
Every case of Peyronie's disease is different. Mr Ollandini will assess your specific situation — phase, curvature, erectile function — and recommend the most appropriate treatment pathway for you.
Myths vs Facts About Peyronie's Disease
Fact: While the acute (active) phase eventually stops progressing and pain often subsides, the fibrous plaque itself rarely disappears without treatment. Most men find their curvature either stabilises or worsens without specific intervention. Waiting without assessment means missing the window for the most effective non-surgical options.
Fact: Peyronie's disease is entirely benign. It is not cancer, it does not become cancer, and it does not increase your risk of developing cancer. The plaque is scar tissue — not a tumour. If you have any concerns about a lump, a specialist assessment will give you clarity and peace of mind.
Fact: While minor or repetitive penile trauma can sometimes trigger the abnormal wound-healing response that leads to Peyronie's, many men develop the condition with no identifiable cause or history of injury. It is a biological disorder of tissue healing — not a consequence of sexual behaviour. There is nothing to feel ashamed about.
Fact: Surgery is reserved for the stable phase and only when curvature significantly impacts sexual function. Many men are successfully managed with non-surgical approaches — including penile traction therapy (PTT), shockwave therapy (Li-ESWT) for pain, and Xiapex® injections where appropriate. The right treatment depends on your individual situation, and a specialist assessment will clarify your options.
Fact: With appropriate treatment, the vast majority of men with Peyronie's disease are able to return to satisfying sexual activity. Whether through non-surgical management, corrective surgery, or penile implant surgery for those with concurrent ED, effective solutions exist. The key is seeking specialist assessment early and not suffering in silence.
Living with Peyronie's: Psychological Impact & Support
Beyond the Physical: It's important to recognise that Peyronie's disease often affects emotional well-being too. Feelings of anxiety, low self-esteem, or depression are common. The condition can also put strain on close relationships and affect sexual function. Dealing with these emotional effects is a key part of good care. Talking openly with your partner and your doctor, considering psychosexual counselling, and connecting with support networks can all help a great deal. Please know, you are not going through this disease alone.

It's vital to recognise that Peyronie's disease impacts more than just physical function. The psychological and emotional consequences can be profound for both the man and his partner:
- Emotional Toll: Anxiety about sexual performance, body image concerns, fear of pain, and worries about relationship impact are common. Studies report significant rates of anxiety and/or depression (up to 48%) among men with Peyronie's.
- Reduced Self-Esteem & Confidence: Changes in penile appearance or function can deeply affect self-worth.
- Relationship Strain: Difficulty with intercourse, avoidance of intimacy, communication breakdowns, and partner concerns can create significant tension.
- Sexual Avoidance: Fear of pain or embarrassment can lead to withdrawal from sexual activity, impacting overall sexual function.
Addressing these dimensions is integral to comprehensive care:
- Open Communication: I encourage open discussion about these sensitive issues during consultations. Talking openly with your partner is also key.
- Partner Involvement: Including partners in the process (with your consent) can be very beneficial.
- Psychosexual Counselling: Specialist therapy offers invaluable tools. I routinely provide referrals to trusted therapists.
- Support Resources: Connecting with others through patient support groups (like online forums associated with the British Dupuytren's Society or international Peyronie's organisations) provides emotional validation and reduces isolation.
These psychological effects can persist even after physical symptoms improve, highlighting the need for ongoing support.
Living with Peyronie's: Long-Term Outlook and Hope
The crucial message is one of hope. While challenging, Peyronie's disease is manageable with appropriate, specialist care. With the right approach – addressing both physical and psychological aspects – most men find significant improvement in function, confidence, and overall quality of life, allowing a return to satisfying intimacy. Effective treatment exists to manage the functional impacts, even if the underlying plaque persists. I've guided many patients through this journey successfully. Remember: it's not life-threatening, not an STI, and not your fault. Expert help is available.
Find help, hope, and understanding.
Why Choose Specialist Urological Care?
The Importance of Expertise: Managing Peyronie's disease well requires a specialist who focuses on men's sexual health (Andrology). Seeing an experienced specialist means you get care based on deep knowledge, access to advanced diagnostic tools, and the full range of modern treatment options — from non-surgical approaches to complex procedures like grafting or penile implants. This expertise allows for truly personalised care plans in a compassionate setting, aimed at achieving the best possible long-term results for your physical function and overall well-being.

Navigating Peyronie's disease benefits significantly from specialist input. Choosing a Consultant Urological Surgeon with a focus on Andrology ensures:
- Specialist Expertise: Deep understanding of the condition's nuances and the underlying disease process.
- Advanced Diagnostics: Proficiency with tools like Penile Doppler Ultrasound.
- Full Range of Treatment Options: Experience across non-surgical and all surgical treatment procedures, including intricate corporoplasty (plication, Nesbit's procedure, plaque incision/grafting) and penile prosthesis implantation (penile implant).
- Personalised Care: Plans tailored to your anatomy, disease phase, goals, and preferences.
- Holistic Approach: Integrating management of psychological and relationship impacts on sexual function.
- Compassionate & Confidential Setting: A supportive and discreet environment for discussing the penis and related concerns.
- Long-Term Management & Follow-up: Commitment to ongoing care.
Take the First Step Towards Recovery and Confidence
Moving Forward: If you've noticed penile curvature, discomfort, lumps, or sexual difficulties, getting expert advice for Peyronie's disease early is the best step you can take. Early assessment often leads to better long-term results and simpler treatment paths. Your consultation will involve careful listening, a thorough assessment, clear explanations of your situation and treatment options, and a collaborative approach to building a personalised plan. Remember, effective management and real improvement are achievable goals for this disease.
Don't delay seeking help if you suspect you have Peyronie's disease. Early assessment, particularly during the acute phase, can make a difference. When you consult with me, you can expect:
- Careful Listening: I take the time to fully understand your history, symptoms, concerns, and goals. Each symptom matters.
- Thorough Examination: A detailed physical assessment is performed.
- Clear Explanations: I explain Peyronie's disease, your specific situation, and all relevant treatment options in understandable terms.
- Open Discussion: All your questions are welcomed and answered comprehensively.
- Collaborative Planning: We work together to create an evidence-based treatment plan tailored to you.
Peyronie's disease can be effectively managed, leading to significant improvements in physical function, sexual confidence, relationship satisfaction, and overall emotional well-being. Taking that first step to seek help is key.
Ready to take control?
Take the first step — book a confidential consultation
You don't have to navigate Peyronie's disease alone. Mr Ollandini provides expert, compassionate care in a completely confidential setting. Most men leave their first consultation feeling significantly reassured and with a clear plan.
How much does treatment actually cost?
Treatment costs vary depending on your individual assessment, the phase of your condition, and the approach recommended. Mr Ollandini is transparent about fees from the outset. Contact the team to discuss pricing before your consultation.
Next Steps
Whether you've just noticed a change or have been living with Peyronie's disease for a while, the right next step is the same: a proper specialist assessment. From there, a personalised plan can be built around your specific situation, goals, and preferences.
References
References for Peyronie's Disease Guide
Terrier JE, Nelson CJ. Peyronie's disease: Contemporary evaluation and management. Int J Urol. 2020;27(6):504-513. doi:10.1111/iju.14230
Nehra A, Alterowitz R, Culkin DJ, et al. Peyronie's Disease: A Review of Etiology, Diagnosis, and Management. J Sex Med. 2015;12(8):1764-1779. doi:10.1111/jsm.12969
Chung E. Peyronie's disease: a literature review on epidemiology, genetics, pathophysiology, diagnosis and work-up. Transl Androl Urol. 2016;5(3):280-289. doi:10.21037/tau.2016.04.05
Carson CC, Hakim LS. Peyronie's Disease: A Review. PMC Journal. 2003;1(2):62-67. doi:10.1111/j.1743-6109.2003.00033.x
Gonzalez-Cadavid NF, Rajfer J. Peyronie's Disease: A Review. J Urol. 2003;169(4):1234-1241. doi:10.1097/01.ju.0000053800.62741.fe
British Association of Urological Surgeons. Information about your penile condition: Peyronie's disease. BAUS Leaflet No: A24/088. Review due: Sep 2026.
Sullivan J, Moskovic D, Nelson C, Levine L, Mulhall J. Prevalence of Peyronie's disease among urologists. J Sex Med. 2015;12(7):1581-1587. doi:10.1111/jsm.12932
Levine LA, Burnett AL. Standard operating procedures for Peyronie's disease. J Sex Med. 2013;10(1):230-244. doi:10.1111/j.1743-6109.2012.03003.x
Ralph D, Gonzalez-Cadavid N, Mirone V, et al. The management of Peyronie's disease: evidence-based 2010 guidelines. J Sex Med. 2010;7(7):2359-2374. doi:10.1111/j.1743-6109.2010.01850.x
Gelbard MK, Dorey F, James K. The natural history of Peyronie's disease. J Urol. 1990;144(6):1376-1379. doi:10.1016/s0022-5347(17)39746-x
Disclaimer: This information is for general educational purposes only and is based on clinical experience and current medical understanding. It should not replace personalised medical advice from a qualified healthcare professional. If you have symptoms that may be related to Peyronie's disease, please see a specialist urologist or other appropriate healthcare provider for a proper diagnosis and tailored treatment recommendations.