As a consultant urological surgeon with a specialist interest in andrology, I regularly see men in clinic who are concerned about how their varicocele relates to their active lifestyle. Perhaps you've noticed a dull ache after lifting weights, wondered whether running is making things worse, or have questions about fertility as someone who trains seriously. These are entirely reasonable concerns, and understanding the relationship between varicocele and physical activity can help you make informed decisions about your health and your training.
This guide is specifically designed for active men—whether you're a competitive athlete, a regular gym-goer, a weekend runner, or someone who simply values staying fit. It builds on the main varicocele information with a focused look at sport-specific considerations, backed by the latest clinical evidence.
If you want a plan, not just information
Train with confidence — and protect fertility if it matters to you.
Train Smarter
what typically triggers ache:
Heavy lifting with breath-holding (Valsalva)
Long cycling sessions (saddle pressure + heat)
High-impact volume (lots of pounding + fatigue)
Know When to Test
when ultrasound / semen analysis adds value
You’re actively trying (or planning) for pregnancy
You’ve noticed testicular size/shape changes
Symptoms are persistent or worsening despite support
A plan you can actually follow
Decide calmly:
When monitoring is sensible
When training modifications are enough
When to discuss embolisation vs surgery around your training cycle
What Happens During The Appointment
- Review symptoms (ache/heaviness, training triggers, fertility goals)
- Examination + grading (including “standing + Valsalva” where appropriate)
- Decide what you actually need: scrotal ultrasound, semen analysis, or reassurance + monitoring
- Clear plan: training modifications, symptom control, and if indicated discussion of embolisation vs microsurgical repair
Recent Development: NICE & Varicocele for Fertility
In September 2025, a draft for the 2026 guidelines revealed that NICE is planning to change its policy on varicocele treatment for infertile men. For years, the UK was the only country where official guidance specifically opposed this treatment, making the shift a significant and long-debated step.
Knowledge check
Quick check: Is it safe to train today?
Select the statement that best describes your situation right now.
Why Varicocele Makes Itself Felt During Sport
Many men with varicocele are entirely unaware they have the condition—until they become more physically active. The relationship between exercise and varicocele symptoms is not coincidental; it reflects the underlying physiology of how blood flows through the spermatic veins.
Is varicocele caused by sport?
The Valsalva Manoeuvre and Its Effects
When you lift something heavy, hold your breath during effort, or strain in almost any way, you naturally perform what's called a Valsalva manoeuvre. This involves closing the glottis (the space between your vocal cords) while attempting to exhale, which dramatically increases pressure in the chest and abdomen.
This pressure surge has several effects on the venous system. It temporarily impedes blood flow returning to the heart, causes engorgement of veins throughout the body, and specifically increases pressure in the testicular venous system. In someone with a varicocele—where the one-way valves in the testicular vein are already failing—this means more blood flows backward and pools in the dilated pampiniform plexus.
Why the Left Side Is Most Affected
You may have noticed that varicoceles almost always occur on the left side (approximately 85-90% of cases). This is due to anatomical factors: the left testicular vein enters the left renal vein at a perpendicular angle, creating greater resistance to flow compared to the right side, where drainage is more direct into the inferior vena cava. During exercise, this anatomical disadvantage becomes more pronounced.
Temperature Effects
Beyond pressure, physical activity also raises scrotal temperature—both through general body heat generation and through the mechanics of clothing and movement. Since the testes rely on being 2-4°C cooler than core body temperature for optimal function, and since varicoceles already impair the normal testicular cooling mechanism, exercise can compound the thermal stress on the testes. This has implications for both comfort and, potentially, for fertility in men who train intensively.
Does Exercise Make Varicocele Worse?
This is one of the most common questions I'm asked in clinic, and the evidence-based answer is nuanced. For most men, regular moderate physical activity does not worsen varicocele or create new ones. However, the intensity and type of exercise do matter—particularly for those with existing varicoceles, and especially when fertility is a consideration.
What science says about it
Common Myths About Exercise and Varicocele
Common Myths About Exercise and Varicocele ✗
Fact
Varicoceles develop due to inherent valve weakness in the testicular veins, often with a genetic component.
Heavy lifting doesn't create varicoceles, but it can make an existing one more noticeable by increasing venous pressure during exertion. Research shows that athletes without any baseline venous reflux develop new varicoceles at approximately the same rate as non-athletes. The apparent connection often arises because men become aware of symptoms during exercise—but the underlying condition was likely already present.
Fact
Reality Most men with varicocele can and should continue exercising. Moderate physical activity is beneficial for overall health and does not typically worsen outcomes. Some modifications may help manage symptoms.
The benefits of regular exercise for cardiovascular health, mental wellbeing, and metabolic function far outweigh the theoretical concerns about varicocele progression in most cases. The key is understanding which activities may require modification and listening to your body.
Fact
Pain is only one consideration. Varicoceles can affect testicular function and fertility even when painless. Men who are concerned about future fertility should consider assessment regardless of symptoms.
The impact on spermatogenesis (sperm production) can occur silently over time, particularly with intensive training that combines mechanical stress with increased scrotal temperature. A painless varicocele in an active man may still warrant monitoring, especially if fertility is a priority.
Fact
Both activities affect varicocele through different mechanisms, and which is "worse" depends on the individual. Running involves impact; cycling involves heat and saddle pressure. Neither is universally more problematic.
The truth is more nuanced: running creates repetitive jarring and may cause mechanical discomfort, while cycling involves prolonged seated position, perineal pressure, and increased scrotal temperature. Different men find different activities more or less tolerable depending on their specific varicocele characteristics.
Key Studies on Exercise and Varicocele Progression
Several studies have examined the relationship between physical activity and varicocele, providing useful clinical guidance:
The Zampieri Longitudinal Study (2011): This three-year study of adolescent boys found that regular sports participation (≥3 times/week) was associated with a significantly higher rate of subclinical varicocele progressing to clinical varicocele (36% vs 5%). However, sports did not increase the development of entirely new varicoceles in boys without baseline reflux.
The Rigano Study: Found that overall varicocele prevalence was not higher in athletes than non-athletes, but athletes with longer weekly training durations (7-12 hours/week) showed higher prevalence and severity than those training less—suggesting a dose-dependent relationship with training volume.
The Aldhafery Survey (2019): Examining 382 athletes in Saudi Arabia, found varicocele prevalence of 46% among screened individuals—higher than the general population rate of approximately 15%. Interestingly, all men with grade 3 varicoceles were training 5 days per week.
Clinical Interpretation
The evidence suggests that while moderate exercise doesn't cause varicoceles, very high training volumes and intensities may accelerate the progression of existing subclinical varicoceles. This has practical implications: if you're training at high intensity and have a known or suspected varicocele, closer monitoring may be warranted. If fertility is a current priority, adjusting training load during the conception period may be beneficial.
Get a Personalised Assessment
Every athlete's situation is different. A specialist consultation includes clinical examination, ultrasound review, and tailored advice for your training goals.
Gym & Weightlifting
Weight training is perhaps the activity most commonly associated with varicocele symptoms, and for good reason. The mechanics of lifting—particularly heavy compound movements—create significant spikes in intra-abdominal pressure that directly challenge the venous return from the testicles.
Varicocele and Gym: a combo everyone talks about
Why Heavy Lifting Affects Varicocele
During heavy lifts, most people instinctively hold their breath and brace their core—the Valsalva manoeuvre. This is actually important for spinal stability and force production, but it creates enormous pressure in the abdominal cavity. Studies have measured intra-abdominal pressures during heavy squats and deadlifts reaching 150-200 mmHg or more—several times higher than resting levels.
This pressure wave reverberates through the venous system. In someone with competent venous valves, this is largely managed. In someone with varicocele, where valves are already failing, this pressure is transmitted directly to the testicular veins, causing further distension and blood pooling.
Exercises Most Likely to Trigger Symptoms
- Deadlifts — Particularly conventional deadlifts with heavy loads. The starting position and the requirement for sustained bracing make this particularly challenging.
- Squats — Both back and front squats, especially when working at high percentages of your maximum. The depth and load combine to create significant pressure.
- Overhead pressing — Standing presses require substantial core bracing, particularly at heavier weights.
- Heavy rows — Bent-over rows and other pulling movements from a hinged position.
- Leg press — Despite being a machine movement, the angle and loading can create substantial abdominal pressure.
Practical Modifications
Consider these evidence-informed strategies if weight training triggers your symptoms:
- Breathing technique: Rather than holding your breath throughout the entire rep, practice exhaling through the sticking point of the lift. This requires practice but can significantly reduce peak pressures while maintaining adequate core stability.
- Rep range adjustment: Working in moderate rep ranges (8-12 reps) at correspondingly lower weights typically generates less peak pressure than very heavy singles or triples, while still providing effective training stimulus.
- Exercise selection: Machine-based alternatives often allow similar muscle targeting with less requirement for extreme bracing. For example, leg extensions and hamstring curls instead of heavy leg press, or chest-supported rows instead of bent-over rows.
- Rest intervals: Longer rest between sets allows symptoms to settle before the next effort. If you're used to 60-90 second rests, try extending to 2-3 minutes on your heavier compound movements.
- Scrotal support: Wearing compression shorts or supportive underwear during training can reduce the mechanical pulling sensation many men experience.
A Note on Bodybuilding and Varicocele Prevalence
Some older literature has reported very high varicocele rates (60-80%) among competitive bodybuilders. While these figures may reflect selection bias in small samples, they highlight that chronic heavy training with sustained Valsalva effort does appear to be associated with higher varicocele prevalence and severity. If you're training at competitive bodybuilding levels and have fertility concerns, earlier intervention on your varicocele may be worth considering.
Running & Endurance Sports
Running affects varicocele through different mechanisms than weight training. Rather than acute pressure spikes, endurance activities create sustained, repetitive stresses that accumulate over time—and introduce the additional factor of increased scrotal temperature during prolonged effort.
If you're a runner with varicocele, you may notice that symptoms are often worse towards the end of longer runs, or in the hours following your session. The repetitive impact of each footstrike creates small mechanical jolts that, over thousands of repetitions, can lead to discomfort. Additionally, the friction and heat build-up from movement raises scrotal temperature—a factor that becomes particularly relevant for fertility.
The good news is that running, unlike heavy lifting, doesn't typically create the extreme pressure spikes that dramatically worsen varicocele during the activity itself. Many runners find they can continue training with relatively minor adjustments. However, for those training at high volumes or with significant fertility concerns, understanding the cumulative effects becomes important.
The Impact Loading Effect
Each footstrike during running generates ground reaction forces typically equivalent to 2-3 times your body weight. This force is transmitted through your skeleton and soft tissues. For someone with a varicocele, this creates a repeated jarring effect on the testicular venous structures—each step is a small mechanical insult that, over the course of a 10km run (approximately 6,000-8,000 footstrikes), can accumulate.
This explains why many runners with varicocele notice symptoms more during the second half of longer runs: the cumulative effect of thousands of impacts eventually overwhelms the body's compensatory mechanisms.
Temperature Considerations
Running generates significant body heat, and the scrotal area is not exempt. Studies have shown that scrotal temperature rises during endurance exercise, and this rise is sustained for as long as activity continues. For runners training for an hour or more, this chronic heat exposure can be relevant:
- The testes require temperatures 2-4°C below core body temperature for optimal spermatogenesis
- Varicocele already impairs the normal counter-current cooling mechanism
- Prolonged running adds an additional thermal stress on top of this baseline impairment
This cumulative thermal effect has more relevance for fertility than for immediate symptoms, but it's worth understanding if you're a high-volume runner with fertility concerns.
Practical Approaches for Runners
- Supportive underwear: Compression shorts or running-specific supportive underwear can reduce mechanical oscillation and the "pulling" sensation many runners describe.
- Hydration: Good hydration helps maintain optimal blood viscosity and venous return. Dehydration thickens blood and may impede drainage.
- Terrain variety: Trail running or grass surfaces reduce impact compared to concrete, potentially lessening cumulative mechanical stress.
- Volume management: If symptoms are problematic, consider whether your training volume could be reduced without significant impact on your goals. Many runners find they can maintain fitness with slightly fewer weekly miles.
- Post-run recovery: Elevating legs after runs, cool showers, and allowing adequate recovery between sessions can help manage symptoms.
Marathon and Ultra-Endurance Considerations
For those training at very high volumes—marathon preparation or ultra-endurance events—the cumulative effects become more significant. Research on endurance athletes has shown transient drops in sperm count and motility after intensive training periods, with recovery typically occurring within days to weeks of reduced training. If you're preparing for a major event and also trying to conceive, timing your training cycles and conception attempts may be worth discussing with your specialist.
Cycling
Cycling presents a unique combination of factors for men with varicocele: prolonged seated positioning, direct saddle pressure on the perineum, and sustained scrotal temperature elevation. For these reasons, cycling deserves special consideration—not necessarily to discourage you from riding, but to help you make informed choices about equipment and technique.
Unlike running or weight training, where the mechanisms are relatively straightforward, cycling's effects on varicocele are multifactorial. The position compresses blood vessels and nerves in the pelvic region. The saddle creates direct pressure on the perineum. And the combination of padded shorts, body heat, and limited airflow creates an environment where scrotal temperature can rise significantly during longer rides.
Saddle Pressure and Venous Congestion
The cycling position—particularly on road bikes with aggressive geometry—places significant weight on the perineum. This area contains blood vessels and nerves that can be compressed during riding. For someone with varicocele, this compression may impede venous drainage from the testicular region, potentially exacerbating venous pooling.
This explains why some cyclists notice varicocele symptoms are different from those experienced in other sports: less of the acute "pulling" sensation, more of a gradual congestion or heaviness that develops over the course of longer rides.
The Heat Factor
Cycling may be the sport with the greatest potential for sustained scrotal temperature elevation:
- Padded cycling shorts, while necessary for comfort, trap heat against the body
- The seated position keeps the scrotum close to the body and the saddle
- Unlike running, there's less natural ventilation from leg movement
- Longer rides (2+ hours) mean prolonged exposure
Research has documented significant scrotal temperature increases during cycling. For men with varicocele—where the normal testicular cooling mechanism is already impaired—this additional heat load can be particularly relevant for fertility considerations.
Practical Strategies for Cyclists
- Saddle selection: Consider saddles with cut-outs or channels designed to relieve perineal pressure. Many modern saddles are designed with this in mind, and finding the right one can significantly improve comfort.
- Bike fit: A professional bike fit can optimise your position to reduce pressure on sensitive areas. Even small adjustments to saddle height, angle, and position can make a meaningful difference.
- Standing intervals: Getting out of the saddle regularly during rides allows blood flow to return to normal and provides relief from sustained pressure.
- Shorts choice: While padding is necessary, some cycling shorts are better ventilated than others. Consider mesh panels or lighter-weight options for warmer conditions.
- Post-ride recovery: Allow time after rides before showering; a cool-down period helps scrotal temperature return to normal. Avoid immediately sitting in a car or continuing to compress the area.
A Positive Note: Horizontal Positioning
It's worth noting that cycling has one advantage over running: when you're on the bike, your body is more horizontal than when standing. This actually reduces the gravitational pooling effect on the varicocele. Some cyclists find that despite the heat and pressure issues, their varicocele is actually less symptomatic during riding than during running. Individual responses vary considerably.
Indoor cycling (turbo trainers, spin bikes) tends to create more scrotal heat than outdoor riding due to the absence of airflow. If you train extensively indoors and have fertility concerns, consider adding a fan directed at your lower body, taking regular breaks, and wearing lighter-weight shorts than you might outdoors.
Hyrox and Hybrid Fitness Competitions
Hybrid endurance–strength events such as Hyrox combine continuous running with repeated high-strain tasks (sled push/pull, wall balls, farmers’ carries, lunges). This creates a physiological pattern highly relevant to men with varicocele.
- Sharp intra-abdominal pressure surges during strength stations — similar to the Valsalva-induced pressure patterns shown to aggravate venous reflux in the spermatic cord.
- Sustained running heat load, which increases scrotal temperature and can magnify the fertility impact of an existing varicocele.
- Repetitive impact and high weekly training volume, echoing athlete profiles in which varicocele progression and more pronounced seminal abnormalities have been documented.
Hyrox does not cause a varicocele in men with normal venous valves, but in those with known or subclinical varicocele, this type of training can:
- Unmask previously silent symptoms
- Worsen post-exercise aching or heaviness
- Accelerate progression from subclinical to clinical varicocele in high-volume athletes
- Compound fertility effects, especially in men training >5 days/week or combining endurance + heavy strength work
Practical recommendations for Hyrox athletes
- Use supportive compression shorts during training and racing to reduce venous pooling.
- Avoid prolonged maximal Valsalva during heavy stations; practise controlled exhalation under load.
- Consider modulating training blocks when trying to conceive, as both varicocele and intense endurance-strength training can impact sperm parameters.
- Seek assessment if training consistently triggers aching, heaviness, or marked asymmetry.
Hyrox is compatible with a healthy lifestyle, but men with known varicocele — or fertility plans — benefit from tailored management and periodic review.
Understanding Pain After Exercise
One of the most characteristic features of varicocele-related discomfort is its timing. Many men tell me they feel fine during their workout, only to notice symptoms appearing and building in the hours afterwards. Understanding why this happens can help you manage your symptoms more effectively and recognise what's normal versus what might warrant concern.
The delayed onset of varicocele symptoms relates to the physiology of venous pooling. During exercise, while pressure may be elevated, blood is also being actively pumped through your system by your working muscles and elevated heart rate. It's once you stop—when muscular pumping ceases and you're upright in normal posture—that pooled blood in the dilated veins becomes most apparent. The gravitational load is now unopposed by active circulation, and the blood that accumulated during exercise takes time to drain.
Typical Symptom Progression
The classic pattern of varicocele symptoms after exercise follows a fairly predictable course:
- During exercise: May be asymptomatic, or may notice mild discomfort with specific movements (particularly heavy lifting or maximal efforts)
- Immediately after: Symptoms begin to emerge as you cool down and return to normal activities
- 1-3 hours post-exercise: Peak symptom intensity often occurs in this window—the characteristic dull ache, heaviness, or pulling sensation
- Evening: Symptoms typically persist or may worsen further if you've been on your feet
- Next morning: Symptoms usually resolve substantially after lying flat overnight
What Research Shows About Pain Intensity
A clinical study by Ebiloglu and colleagues quantified the relationship between exercise and varicocele pain. Among men with painful varicoceles, engaging in continuous physical activity caused mean pain scores to spike from approximately 3/10 at baseline to 7.5/10 post-exertion. This objective measurement confirms what many men experience subjectively—that exercise significantly amplifies varicocele discomfort.
Importantly, the same study showed that surgical treatment (varicocelectomy) was highly effective at resolving this exercise-induced pain, with microsurgical repair providing essentially complete relief in most cases.
Strategies for Managing Post-Exercise Symptoms
- Cool shower or bath: Cooling the scrotal area helps with vasoconstricton and symptom relief. Avoid hot showers immediately post-exercise.
- Elevation: Lying down with legs elevated for 10-15 minutes after exercise allows drainage and reduces symptoms.
- Supportive underwear: Continuing to wear supportive compression shorts in the hours after exercise can help.
- Gentle movement: Paradoxically, remaining completely sedentary can worsen symptoms. Light walking promotes venous return.
- Timing awareness: Plan activities requiring you to be on your feet for extended periods (standing events, long meetings) for days when you haven't trained heavily.
When to Stop Training and Seek Assessment
Seek Urgent Medical Attention
- Sudden, severe testicular pain (could indicate torsion—an emergency)
- Nausea or vomiting with testicular pain
- Testicle appears higher than usual or rotated
- Rapid-onset swelling, especially if painful
- Pain with fever or urinary symptoms
Continue Training (With Awareness)
- Gradual, dull ache that improves with rest
- Symptoms that follow the typical post-exercise pattern
- Discomfort that resolves overnight
- Heaviness without sharp or severe pain
- Symptoms consistent with previous episodes
- Zampieri N, Dall'Agnola A. Subclinical varicocele and sports: a longitudinal study. Urology. 2011;77(5):1199-1202.
- Di Luigi L, et al. Physical activity as a possible aggravating factor for athletes with varicocele: impact on the semen profile. Hum Reprod. 2001;16(6):1180-1184.
- Ebiloglu T, et al. The effect of physical activity on varicocele pain and resolution of this pain by different varicocelectomy techniques. Can J Urol. 2016;23(3):8285-8290.
- Aldhafery BF, et al. Prevalence and awareness of varicocele among athletes in Riyadh, Saudi Arabia. Res Rep Urol. 2019;11:231-238.
- Oranges F, et al. The Influence of an Intense Training Regime in Professional and Non-Professional Athletes on Semen Parameters: A Systematic Review. J Clin Med. 2025;14(1):201.
- Radojević N, et al. Restricting sports activity in reducing the rate of varicocele and related infertility parameters in athletes. Arch Med Sci. 2015;11(1):169-173.
- Practice Committee of the American Society for Reproductive Medicine. Report on varicocele and infertility: a committee opinion. Fertil Steril. 2020;114(6):1135-1142.
- NICE Clinical Knowledge Summaries: Male Infertility. Updated 2024.
Fertility Considerations for Athletes
For men who are active and also concerned about current or future fertility, the relationship between varicocele, exercise, and reproductive health deserves careful attention. The evidence suggests that intensive training may compound the negative effects of varicocele on sperm parameters—but also that these effects are often reversible with appropriate intervention.
Varicocele is the most common correctable cause of male infertility, affecting approximately 40% of men presenting with primary infertility. In athletes, the situation may be more complex: the combination of mechanical stress, thermal load, and oxidative stress from intense training can amplify the impact of varicocele on spermatogenesis beyond what would be expected from either factor alone.
The "Double Hit" Effect
Research by Di Luigi and colleagues demonstrated that athletes with varicocele showed significantly worse sperm parameters (motility, morphology) than sedentary men with equivalent varicoceles. The effect was not simply additive—intense exercise appeared to amplify the negative impact of varicocele on reproductive function. This suggests that very active men with varicocele may face a compounded fertility risk.
Heat, Oxidative Stress, and Sperm DNA Fragmentation
Three interconnected mechanisms explain how exercise and varicocele combine to affect fertility:
Thermal stress: Spermatogenesis is exquisitely sensitive to temperature. The testes evolved to sit outside the body cavity specifically because they require temperatures 2-4°C below core body temperature for optimal function. Varicocele impairs the normal counter-current cooling mechanism of the testicular blood supply. Intensive exercise—particularly endurance sports and cycling—adds an additional heat load. The combination can create sustained periods of elevated testicular temperature that impair sperm production and quality.
Oxidative stress: Intense exercise generates reactive oxygen species (ROS) throughout the body as a byproduct of high metabolic activity. While the body has antioxidant defences, these can be overwhelmed during very heavy training. Varicocele independently increases oxidative stress in the testicular environment through hypoxia and venous stasis. Athletes with varicocele may therefore experience a "double hit" of oxidative damage to their sperm.
Sperm DNA fragmentation: Both heat and oxidative stress can damage sperm DNA. High DNA fragmentation index (DFI) is associated with reduced natural conception rates and poorer IVF/ICSI outcomes. Research has shown that varicocele repair can reduce sperm DNA fragmentation, suggesting this mechanism is treatable.
What the Studies Show
The Di Luigi Study: This pivotal research compared four groups: athletes and non-athletes, with and without varicocele. Key findings:
- Athletes with varicocele had lower progressive sperm motility than non-athletes with varicocele
- Morphologically normal sperm percentage was approximately 34% in athletes with varicocele versus 42% in non-athletes with varicocele
- Only the athletic varicocele group showed significant testicular volume discrepancy (left hypotrophy)—a marker of varicocele-induced testicular damage
- Importantly, resting hormone levels were similar across groups, suggesting local testicular effects rather than systemic hormonal disturbance
The Radojević Study: Adolescent athletes with varicocele who stopped sports for six months showed:
- Significant improvements in sperm concentration and motility
- Complete resolution of varicocele in 18 out of 49 athletes
- One-grade improvement in varicocele in a further 19 athletes
This study provides particularly valuable evidence that training-related varicocele effects can be at least partially reversible.
Clinical Implications for Active Men
For athletes with varicocele who are concerned about fertility, several evidence-based strategies emerge:
- Earlier consideration of varicocele repair: Given the compounded effect of intense training on varicocele-related fertility impairment, proactive treatment may be particularly beneficial in very active men.
- Training load modification during conception attempts: Temporarily reducing training intensity and volume while trying to conceive may improve sperm parameters. This is a time-limited intervention that need not permanently affect your athletic goals.
- Heat management: Specific attention to scrotal cooling—avoiding hot baths, using cooling strategies during indoor training, choosing lighter shorts—may help protect sperm production.
- Antioxidant consideration: While the evidence for antioxidant supplements is mixed, some specialists recommend them for active men with varicocele and fertility concerns. Discuss this with your treating physician.
- Semen analysis monitoring: Regular semen analysis (every 6-12 months) allows tracking of any changes and informs decisions about timing of intervention.
The NICE Guidelines Shift
It's worth noting that NICE has recently produced a draft for their new guidelienes 2026 with an important update. In its guidance NICE acknowledge a role for varicocele repair in men with abnormal semen parameters and clinical varicocele. This represents a significant shift from previous, more conservative guidance and reflects growing recognition that varicocele treatment can meaningfully improve fertility outcomes. For athletes with varicocele and fertility concerns, this supports earlier discussion of treatment options.
Knowledge check
Which factor does NOT typically contribute to reduced fertility in athletes with varicocele?
Knowledge check
Research suggests that when athletes with varicocele stop intensive training for six months:
Fertility Concerns?
Semen analysis and fertility assessment available as part of your consultation. Let's discuss your options while you continue training.
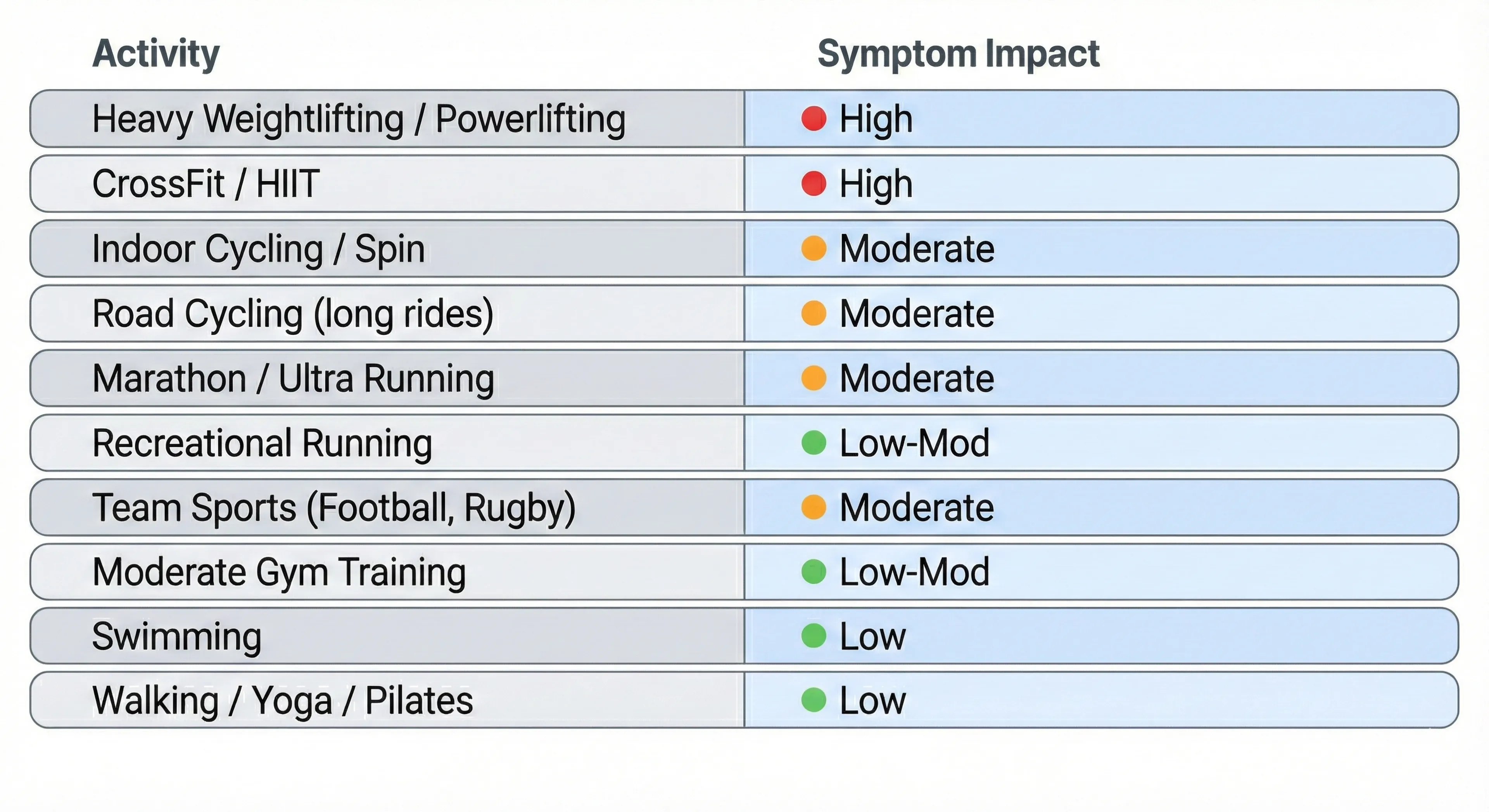
Sports Impact Index
Not all sports affect varicocele equally. The following index provides a general guide to how different activities tend to influence symptoms and fertility considerations. Remember that individual responses vary considerably—some men tolerate activities that others find problematic.
Did you know?
Interestingly, research suggests swimming may actually be protective against varicocele development and progression. A study comparing water-polo players to other athletes found that the aquatic group had a lower incidence of varicocele (approximately 9%) than even the non-athlete control group (approximately 12%).
Why Swimming May Be Beneficial
- Horizontal positioning: Swimming reduces gravitational pooling in the scrotal veins
- Water cooling: Immersion in water (especially cooler water) keeps scrotal temperature low
- No Valsalva strain: Swimming involves minimal breath-holding under strain compared to weight training
- Hydrostatic pressure: Water pressure may actually assist venous return
For men with varicocele who want to maintain high fitness levels while minimising symptom aggravation, swimming can be an excellent option. Many patients report that it's one of the few vigorous activities that doesn't worsen their symptoms—and some find it actually provides relief.1
When to Seek Specialist Assessment
While many men with varicocele successfully manage their symptoms alongside an active lifestyle, there are circumstances where specialist assessment becomes particularly valuable. As a urologist with a focus on andrology, I see patients across a spectrum—from those seeking reassurance that their approach is sound, to those requiring intervention to protect their fertility or quality of life.
Assessment is particularly worthwhile when symptoms begin to interfere with training enjoyment or consistency, when fertility is a current or future priority, or when you've noticed changes that concern you. A specialist consultation typically involves clinical examination, ultrasound imaging, and—where relevant—semen analysis, providing a complete picture of your individual situation.
When to Seek Specialist Assessment
While many men with varicocele successfully manage their symptoms alongside an active lifestyle, there are circumstances where specialist assessment becomes particularly valuable. As a urologist with a focus on andrology, I see patients across a spectrum—from those seeking reassurance that their approach is sound, to those requiring intervention to protect their fertility or quality of life.
Assessment is particularly worthwhile when symptoms begin to interfere with training enjoyment or consistency, when fertility is a current or future priority, or when you've noticed changes that concern you. A specialist consultation typically involves clinical examination, ultrasound imaging, and—where relevant—semen analysis, providing a complete picture of your individual situation.
Not sure if your symptoms warrant assessment?
Many athletes I see weren't sure either. A consultation clarifies whether you need intervention or can continue training with modifications — and gives you a clear plan either way.
Return to Sport After Varicocele Treatment
For athletes who undergo varicocele repair—whether microsurgical varicocelectomy or embolisation—a key question is how quickly and safely they can return to training. The good news is that modern techniques allow relatively rapid recovery, and most men are back to full activity within four to six weeks.
The recovery timeline depends somewhat on the procedure performed (surgical versus embolisation) and the intensity of sport you plan to return to. What follows is a general framework; your surgeon's specific instructions should take precedence, as they're tailored to your individual procedure and circumstances.

Plan your surgery around your competition calendar
Detailed Recovery Guidance
Microsurgical Varicocelectomy Recovery
Microsurgical inguinal or subinguinal varicocelectomy involves a small incision in the groin and meticulous ligation of the dilated veins under magnification. Recovery is generally straightforward:
- Mild scrotal swelling and discomfort typically resolves within days
- Incision heals over 10-14 days; sutures are usually dissolvable
- Most patients can return to sedentary work within a week
- Full recovery for sport is typically achieved by 4-6 weeks
Embolisation Recovery
Varicocele embolisation is performed by an interventional radiologist, accessing the testicular vein through a small puncture in the neck or groin. Recovery is often faster than surgery:
- No groin incision means less initial discomfort
- Many patients return to light activity within days
- Light exercise often permitted within 1-2 weeks
- Full return to sport may be possible by 3-4 weeks
However, embolisation carries a slightly higher recurrence rate than microsurgical repair in some studies. Your surgeon can advise on the most appropriate procedure for your circumstances.
Sport-Specific Considerations
Weightlifting: The exercises most affected by varicocele—heavy compounds with Valsalva—should be the last to return to your programme. Start with machines and lighter loads, progressing over 2-3 weeks once cleared for full training.
Running: Usually can resume jogging by week 3-4, progressing to normal running by week 5-6. Impact may cause mild awareness of the surgical area initially; this typically resolves quickly.
Cycling: Once wounds are fully healed (typically by week 3), cycling can resume. Start with shorter rides and ensure saddle comfort before returning to longer distances.
Contact sports: Wait until 6 weeks or until cleared by your surgeon. Wearing a protective cup is advisable for the first few months after return.
What to Expect After Recovery
Most athletes report that the exercise-induced symptoms they experienced before surgery are substantially or completely resolved after varicocelectomy. In the Ebiloglu study, microsurgical repair resulted in essentially complete pain relief (mean VAS scores below 1/10) in most patients. This means you can often train more effectively after treatment, without the limitation of varicocele-related discomfort.
For fertility, improvements in semen parameters typically become apparent around 3 months post-operatively, reflecting the full spermatogenic cycle. Follow-up semen analysis at 3-6 months allows assessment of any improvement.
Practical Strategies for Training with Varicocele
Whether you're managing symptoms while awaiting treatment, have decided on conservative management, or simply want to train as comfortably as possible, the following evidence-informed strategies can help you continue enjoying physical activity with varicocele.
Key Principles
- Support: Reducing mechanical stress on the varicocele
- Technique: Minimising unnecessary pressure during exertion
- Cooling: Managing scrotal temperature, particularly for fertility
- Recovery: Optimising drainage after exercise
- Awareness: Recognising what's normal and what warrants attention
Supportive Underwear and Compression
Appropriate support can significantly reduce the mechanical "pulling" sensation many men experience during exercise:
- Compression shorts: Purpose-designed athletic compression shorts provide support without being restrictive. Look for quality materials with adequate elasticity.
- Jockstrap: Traditional athletic supporters remain an effective option, particularly for high-impact activities or when extra support is needed.
- Running shorts with liner: Built-in brief liners provide some support; consider layering with compression shorts for longer runs if symptoms are problematic.
- Avoid loose underwear during exercise: Standard boxers provide minimal support and allow the varicocele to move freely—not ideal during physical activity.
Breathing and Technique for Weight Training
- Practice controlled exhale: Rather than holding your breath throughout heavy lifts, practice exhaling through the sticking point. This takes practice but can meaningfully reduce peak intra-abdominal pressure.
- Avoid prolonged breath-holds: Multiple reps without breathing creates sustained pressure. Breathe between reps.
- Consider a belt strategically: Weight belts can actually increase intra-abdominal pressure (that's partly their purpose). Consider whether you truly need one, or whether it's exacerbating symptoms.
- Exercise selection: Where possible, substitute exercises that require less extreme bracing. Machines often allow similar targeting with reduced pressure demands.
Temperature Management (Particularly for Fertility)
- Avoid hot baths/saunas post-exercise: A cool or lukewarm shower is preferable. Hot immersion adds thermal stress when the testes are already warmed from exercise.
- Indoor training considerations: Add a fan directed at your lower body during indoor cycling or gym sessions. The absence of outdoor airflow means heat accumulates more rapidly.
- Clothing choice: Looser, lighter-weight shorts may be preferable to heavily padded or tight options, particularly in warm conditions. Balance support needs with ventilation.
- Post-exercise cooling: Allow time in a cool environment after training before showering or sitting. This helps scrotal temperature return to normal.
Post-Exercise Recovery Strategies
- Elevation: Lying down with legs elevated for 10-15 minutes after exercise promotes venous drainage and can reduce post-exercise symptoms.
- Cool shower: Cooling the scrotal area helps with vasoconstriction and symptom relief.
- Gentle movement: Complete immobility after exercise can actually worsen venous pooling. Light walking in the hours after training helps maintain circulation.
- Adequate rest days: If symptoms are significant, ensure you're allowing adequate recovery between sessions. Chronic accumulated stress may be worse than any single session.
Training Programme Adjustments
- Volume vs intensity: If symptoms are problematic, consider whether you can achieve your goals with slightly lower intensity and higher volume, reducing peak pressure demands.
- Exercise order: Front-loading your most challenging exercises when you're fresh, rather than leaving heavy compounds until you're fatigued, may reduce total stress.
- Activity variety: Incorporating lower-impact activities (swimming, cycling with good saddle setup) alongside higher-impact training can maintain fitness while providing symptom relief days.
- Fertility-focused timing: If actively trying to conceive, consider timing your highest-volume training blocks for periods when conception is not being attempted, and moderating training during fertility windows.
Athlete timeline: training and recovery
- If no procedure: you usually keep training with modifications + support garments
- If embolisation/surgery considered: we discuss time off heavy lifting, return-to-running, and what to do during the fertility window
- If fertility is the priority: we align testing and timing (semen analysis trend matters more than panic)
This guide has been shaped by the concerns and experiences patients have shared with me in clinic over the years. The questions you ask—whether about training modifications, fertility implications, or recovery timelines—directly inform what I include and how I explain it. If you have questions this page hasn't answered, or if your experience with varicocele and sport offers insights that might help others, I'd genuinely value hearing from you.
Ask a Question
If something on this page is unclear, or if you have a question I haven't addressed, you're welcome to get in touch. While I can't provide individualised medical advice without a proper consultation—your specific situation requires proper assessment—questions that might help other readers may be incorporated into future updates to this page.
Common themes from patient questions have already shaped sections on post-exercise pain timing, the "myths versus facts" clarifications, and the sport-specific practical modifications. Your question might help the next person seeking the same information.
Share Your Experience
If you've navigated varicocele as an active person—whether managing symptoms conservatively, modifying your training approach, or returning to sport after treatment—your experience could help others feel less alone with this condition.
Many men tell me they felt isolated when first researching varicocele and sport, uncertain whether their symptoms were normal or whether their concerns were valid. Hearing from others who've been through similar experiences can be genuinely reassuring.
I'm considering adding an anonymous patient experiences section in future updates to this guide. If you'd be interested in contributing a brief account of your journey—what worked, what didn't, what you wish you'd known earlier—please let me know.
Was This Guide Helpful?
Feedback helps me understand what's working and what could be improved. If this guide has answered your questions, helped you make decisions about your training or treatment, or simply reassured you that your concerns are valid, I'd appreciate knowing.
Equally, if you found sections confusing, felt important topics were missing, or think the tone didn't quite land, constructive feedback helps me serve future readers better.
You can reach me through the contact form on this website, or mention this page when booking a consultation if you'd like to discuss your situation in more depth.
A Note on Online Discussions
I'm aware that varicocele is actively discussed on social media platforms and forums, with men sharing experiences, concerns, and sometimes conflicting advice. Some of these discussions raise valid questions; others promote treatments with limited evidence or generate unnecessary anxiety.
If you've come to this page after reading worrying posts elsewhere—perhaps about exercise "destroying" fertility or varicocele being a "silent threat"—I hope the evidence-based perspective here has been helpful. The reality is usually more nuanced than alarming headlines suggest, and most men with varicocele can continue enjoying active lifestyles with appropriate awareness and, where needed, effective treatment.
Practice Transparency: Fees and Prices
Radical transparency means that I will always be clear and upfront about the costs and the fees you are going to face.
LIMITATIONS AND UNCERTAINTIES
What We Don't Yet Know: Limitations of the Evidence
As with all areas of medicine, our understanding of varicocele and sport is evolving. I believe in being transparent about what the research tells us with confidence and where genuine uncertainty remains.
Most studies examining varicocele and exercise are observational rather than randomised controlled trials. This means we can identify associations—for instance, that athletes with varicocele have worse semen parameters than non-athletes with varicocele—but we cannot definitively prove that exercise caused the difference. There may be confounding factors we haven't fully accounted for.
The Zampieri longitudinal study is one of the few that followed participants prospectively over time, providing stronger evidence for a causal relationship between sports participation and varicocele progression. However, it focused on adolescents rather than adult athletes, and we cannot assume findings translate directly across age groups.
Sample sizes in many studies are relatively small, and populations studied (often young men in specific countries or sports) may not fully represent the diversity of men seeking guidance.
The impact ratings I've presented synthesise evidence from multiple sources, including peer-reviewed studies, clinical experience, and patient reports. They are not derived from a single definitive study comparing all activities head-to-head under identical conditions—no such study exists.
Individual responses vary considerably. Some men tolerate activities I've rated as "high impact" with minimal symptoms, while others find "low impact" activities unexpectedly problematic. Your anatomy, varicocele grade, baseline fitness, training technique, and numerous other factors all influence your personal response.
The ratings should guide initial thinking and inform conversations with your clinician—they should not be interpreted as absolute restrictions. If an activity feels comfortable and isn't interfering with your goals, the classification on a general index matters less than your lived experience.
While we have reasonable evidence that varicocele affects semen parameters and that intense exercise can compound this effect, long-term conception outcomes in athletes with treated versus untreated varicoceles remain less well-studied than we'd like.
Most fertility research uses semen parameters—sperm count, motility, morphology, and sometimes DNA fragmentation—as surrogate endpoints rather than actual pregnancy rates. These parameters correlate with fertility but don't perfectly predict it. A man with moderately impaired parameters may conceive without difficulty; another with better numbers may struggle. The relationship is probabilistic rather than deterministic.
The optimal timing of varicocele treatment relative to training cycles, the magnitude of benefit from temporary training reduction during conception attempts, and the interaction between varicocele treatment and assisted reproduction outcomes all warrant further research.
Several questions remain genuinely unsettled in the literature:
Whether swimming is truly protective against varicocele or simply neutral compared to sedentary controls. The water-polo study is intriguing but represents a single observation that requires replication.
The exact threshold of training volume or intensity where risk becomes clinically significant. Current evidence suggests a dose-response relationship, but we cannot specify precise cut-offs with confidence.
Whether temporary training reduction during conception attempts independently improves outcomes, or whether its benefit is primarily mediated through allowing varicocele treatment and recovery.
The relative contribution of heat, oxidative stress, mechanical factors, and hormonal fluctuations to exercise-related fertility effects—and whether targeting specific mechanisms (for instance, with cooling strategies or antioxidants) can meaningfully mitigate risk.
These limitations don't mean the guidance on this page is unreliable. The core principles—that intense exercise can unmask or accelerate existing varicoceles, that symptoms characteristically worsen after activity, that fertility effects may compound in very active men, and that treatment is highly effective—are well-supported by consistent evidence across multiple studies.
However, the limitations underscore why individualised assessment matters. Your specific situation may differ from study populations in important ways. Decisions about monitoring, training modification, or treatment should be made collaboratively with a specialist who understands both the evidence and your personal circumstances, goals, and values.
If you're uncertain how to weigh the evidence in your situation, or if you'd like to discuss what these limitations mean for your specific case, I'm happy to explore them during a consultation.
FAQs
For most men, moderate exercise does not worsen varicocele in terms of progression or long-term outcomes. However, certain high-intensity activities—particularly heavy weightlifting with Valsalva—can make symptoms more noticeable and may accelerate the progression of existing subclinical varicoceles in some cases. The key distinction is between experiencing symptoms during/after exercise (which is common and manageable) versus actually worsening the underlying condition (which requires more intensive training over longer periods to occur). General fitness activities are not harmful and have many benefits that outweigh any theoretical varicocele concerns.
The decision about varicocele surgery depends on your symptoms, fertility concerns, and personal circumstances—not specifically on whether you're an athlete. However, if symptoms are significantly interfering with training, or if you're concerned about fertility while continuing high-intensity exercise, treatment may be particularly beneficial. The recovery period (4-6 weeks) is relatively short, and most athletes report improved comfort and ability to train after successful repair. This is a decision best made with specialist advice tailored to your situation. Should I have varicocele surgery if I'm an athlete?
Most men can return to light gym activity by 2-3 weeks post-operatively, with progression to full training by 4-6 weeks. Heavy compound lifts (deadlifts, squats) should be the last exercises reintroduced. Always follow your surgeon's specific guidance, as individual circumstances vary. The good news is that most athletes find their varicocele-related symptoms are substantially or completely resolved after successful surgery, often allowing better training than before.
Varicocele is the most common correctable cause of male infertility, and research suggests that intense athletic training may compound its negative effects on semen parameters. The mechanisms involve heat, oxidative stress, and mechanical factors. Importantly, these effects are often reversible: treatment of varicocele typically improves semen parameters, and temporary reduction in training intensity during conception attempts may also help. For athletes with fertility concerns, proactive assessment and management is worthwhile.
Rather than "avoid," I'd suggest being thoughtful about exercises that create high intra-abdominal pressure: heavy deadlifts, squats, leg press, and standing overhead press are the main ones. Many men can continue these with modifications (breathing technique, moderate loads, adequate rest intervals). Machine-based alternatives often allow similar muscle targeting with less pressure demand. The goal isn't necessarily to eliminate exercises, but to modify your approach so symptoms are manageable.
Post-exercise symptoms are characteristic of varicocele. During activity, blood is actively pumped through your system; once you stop, the muscular pumping ceases and blood that accumulated in the dilated veins during exercise takes time to drain. The gravitational load is now unopposed, leading to the typical dull ache or heaviness. Symptoms tend to peak 1-3 hours post-exercise and usually resolve overnight. Elevation, cool showers, and supportive underwear can help manage this pattern.
Cycling doesn't cause varicocele, but it presents specific challenges for men who have one: saddle pressure, heat accumulation, and prolonged seated positioning. The impact tends to be more on fertility (through sustained scrotal temperature elevation) than on symptoms. Good saddle choice, proper bike fit, standing intervals, and adequate ventilation can make cycling comfortable and reduce any impact. Many cyclists with varicocele continue to ride successfully with appropriate equipment modifications.
Varicocele doesn't directly affect athletic performance in the way an injury to a muscle or joint would. However, if symptoms are distracting or limiting your ability to train as you'd like, this could indirectly affect your progress and enjoyment of sport. Some men also report a psychological impact from concern about their condition. Treatment of symptomatic varicocele typically allows full return to training without limitation, often with improved comfort.
This guide synthesises evidence from peer-reviewed research, clinical guidelines, and my experience treating active men with varicocele. Below are the key studies informing the guidance on this page, organised by topic.
Physical Activity and Varicocele Progression
Zampieri N, Dall'Agnola A. Subclinical varicocele and sports: a longitudinal study. Urology. 2011;77(5):1199-1202. This three-year prospective study followed adolescent boys and found that regular sports participation (three or more times weekly) was associated with a significantly higher rate of subclinical varicocele progressing to clinical varicocele (36% versus 5%). Crucially, sports did not increase the development of entirely new varicoceles in boys without baseline reflux—suggesting exercise unmasks rather than creates varicoceles.
Rigano E, Santoro G, Impellizzeri P, et al. Varicocele and sport in adolescents: a preliminary report. J Endocrinol Invest. 2004. Found that overall varicocele prevalence was not higher in athletes than non-athletes, but athletes with longer weekly training durations (7-12 hours per week) showed higher prevalence and severity than those training less—suggesting a dose-dependent relationship with training volume.
Athletes, Varicocele and Fertility
Di Luigi L, Gentile V, Pigozzi F, Parisi A, Giannetti D, Romanelli F. Physical activity as a possible aggravating factor for athletes with varicocele: impact on the semen profile. Hum Reprod. 2001;16(6):1180-1184. This pivotal study compared four groups: athletes and non-athletes, with and without varicocele. Athletes with varicocele had significantly worse sperm motility and morphology than non-athletes with equivalent varicoceles. Only the athletic varicocele group showed significant testicular volume discrepancy—a marker of varicocele-induced testicular damage.
Radojević N, Lazović JM, Šantrić V, et al. Restricting sports activity in reducing the rate of varicocele and related infertility parameters in athletes. Arch Med Sci. 2015;11(1):169-173. Adolescent athletes with varicocele who stopped sports for six months showed significant improvements in sperm concentration and motility, with complete resolution of varicocele in 18 out of 49 athletes and one-grade improvement in a further 19. This provides evidence that training-related varicocele effects can be at least partially reversible.
Oranges F, Mirone V, Verze P, et al. The Influence of an Intense Training Regime in Professional and Non-Professional Athletes on Semen Parameters: A Systematic Review. J Clin Med. 2025;14(1):201. This recent systematic review confirmed that intensive training regimes can negatively affect semen parameters through mechanisms including oxidative stress, elevated scrotal temperature, and hormonal fluctuations—effects that may compound existing varicocele-related impairment.
Pain and Physical Activity
Ebiloglu T, Kaya E, Köprü B, Topuz B, Irfanoğlu ME, Kibar Y. The effect of physical activity on varicocele pain and resolution of this pain by different varicocelectomy techniques. Can J Urol. 2016;23(3):8285-8290. Quantified the relationship between exercise and varicocele pain: among men with painful varicoceles, continuous physical activity caused mean pain scores to spike from approximately 3/10 at baseline to 7.5/10 post-exertion. Microsurgical varicocelectomy provided essentially complete pain relief in most cases.
Athlete Prevalence and Awareness
Aldhafery BF, Alzerwi NA, Aldhuayan AA, et al. Prevalence and awareness of varicocele among athletes in Riyadh, Saudi Arabia. Res Rep Urol. 2019;11:231-238. Examined 382 athletes and found varicocele prevalence of 46%—substantially higher than the general population rate of approximately 15%. All men with grade 3 varicoceles were training five days per week. Awareness of varicocele among athletes was low, with only 31% having heard of the condition and just 12% understanding its potential fertility implications.
Swimming and Aquatic Sports
Di Luigi L, et al. (Study comparing water-polo players to other athletes) Found that water-polo players had a lower incidence of varicocele (approximately 9%) than even non-athlete controls (approximately 12%), suggesting potential protective effects from horizontal positioning, water cooling, absence of Valsalva strain, and hydrostatic pressure assisting venous return.
Clinical Guidelines
Practice Committee of the American Society for Reproductive Medicine. Report on varicocele and infertility: a committee opinion. Fertil Steril. 2020;114(6):1135-1142. Current ASRM guidance on varicocele assessment and treatment in the context of male infertility.
European Association of Urology. Guidelines on Male Infertility. 2024. European clinical recommendations for varicocele management.
NICE Clinical Knowledge Summaries. Male Infertility. Updated 2024. UK national guidance, with significant draft updates expected in 2026 regarding varicocele treatment for fertility.
Background Reading
Shi M, Zhang Y, Zhang X, et al. Risk factors associated with varicocele: a narrative review. Transl Androl Urol. 2024;13(5):819-830. Comprehensive overview of varicocele risk factors including anatomical, genetic, and lifestyle factors.
The Sports Impact Index presented on this page synthesises evidence from multiple sources. For transparency, here is the specific evidence underpinning each rating:
High Impact Activities
Heavy Weightlifting / Powerlifting and CrossFit / HIIT: Rated high based on the Valsalva mechanism generating intra-abdominal pressures of 150-200 mmHg during heavy lifts, the Di Luigi study demonstrating compounded fertility effects in athletes with varicocele, and older literature reporting 60-80% varicocele prevalence in competitive bodybuilders (though these figures may reflect selection bias). The Aldhafery study's finding that all grade 3 varicoceles occurred in men training five days weekly supports a dose-response relationship with intense training.
Moderate Impact Activities
Indoor Cycling / Spin: Rated moderate based on heat accumulation without outdoor airflow, saddle pressure on perineum, and prolonged seated positioning. Specific comparative studies are limited; rating extrapolated from general cycling research on perineal pressure and scrotal temperature studies.
Road Cycling (long rides): Rated moderate based on multiple studies documenting sustained scrotal temperature elevation during cycling, perineal pressure effects, and prolonged seated position. Partially offset by the horizontal positioning advantage and outdoor airflow.
Marathon / Ultra Running: Rated moderate based on the Zampieri longitudinal study (36% versus 5% progression in active versus sedentary adolescents) and cumulative impact loading over thousands of footstrikes. The Di Luigi study confirmed semen parameter effects in endurance athletes.
Team Sports (Football, Rugby): Rated moderate based on the Aldhafery study showing 46% varicocele prevalence among athletes with higher grades associated with greater training frequency. Combines elements of impact, exertion, and variable intensity.
Low to Moderate Impact Activities
Recreational Running: Rated low-moderate based on the Zampieri study showing lower progression rates with moderate training frequency (fewer than three times weekly) compared to intensive training.
Moderate Gym Training: Rated low-moderate based on the Rigano study finding overall prevalence not elevated in athletes, with dose-dependent effects only apparent at higher training volumes.
Low Impact Activities
Swimming: Rated low based on the study of water-polo players showing approximately 9% varicocele incidence versus approximately 12% in non-athlete controls, suggesting possible protective effect. Mechanisms include horizontal positioning reducing gravitational pooling, water cooling maintaining scrotal temperature, absence of Valsalva strain, and hydrostatic pressure potentially assisting venous return.
Walking / Yoga / Pilates: Rated low based on minimal intra-abdominal pressure generation, absence of impact loading, and no significant heat accumulation. No studies directly examining varicocele impact; ratings derived from physiological principles.
Important Caveat
These ratings represent synthesis across heterogeneous studies with varying methodologies, populations, and endpoints. No single study has directly compared all activities head-to-head in a randomised controlled design. Individual responses vary considerably, and these ratings should inform initial thinking rather than dictate absolute restrictions. Clinical decisions should be individualised based on your specific symptoms, varicocele grade, fertility priorities, and training goals.
Understanding your options and knowing where to find reliable information empowers you to make informed decisions about your health. Below are resources I recommend, organised by category.
GGO Med Resources
If you'd like to explore related topics in more depth, the following pages on this website may be helpful:
Our comprehensive Varicocele Guide covers diagnosis, grading, treatment options, and what to expect from surgery or embolisation in detail. If you're considering treatment, this provides the complete picture.
The Male Fertility Overview explains the broader context of reproductive health, including how varicocele fits alongside other factors affecting fertility.
Professional Clinical Guidelines
For those who want to see the source guidance that informs clinical practice:
NICE Clinical Knowledge Summaries on Male Infertility provides UK national guidance. Note that significant updates regarding varicocele treatment are expected in the 2026 guidelines, with draft documents already suggesting a shift toward greater support for intervention in appropriate cases.
The European Association of Urology Guidelines on Male Infertility offer comprehensive European clinical recommendations, updated regularly based on emerging evidence.
The American Urological Association and American Society for Reproductive Medicine both publish guidance documents that, while US-focused, reflect international expert consensus on varicocele management.
Fertility Support Organisations
If fertility concerns are part of your picture, these organisations offer information, support, and community:
Fertility Network UK is the leading UK charity supporting anyone facing fertility challenges. They offer information resources, support groups, and a helpline staffed by trained volunteers who understand what you're going through.
The Human Fertilisation and Embryology Authority (HFEA) is the UK regulator for fertility treatment. Their website includes a clinic finder, treatment success rate data, and comprehensive information about assisted reproduction options.
Fertility Friends provides online forums where you can connect with others facing similar challenges. Sometimes knowing you're not alone is as valuable as clinical information.
The Donor Conception Network offers specific support for those considering or using donor conception as part of their family-building journey.
Men's Health Resources
For broader men's health information and support:
The Men's Health Forum works to improve men's health through research, advocacy, and direct support services.
Prostate Cancer UK, while focused primarily on prostate conditions, offers excellent resources on urological health more broadly and advocates for better men's health services.
Research and Evidence
If you're interested in reading the primary research yourself:
PubMed provides free access to abstracts and many full-text articles. Searching "varicocele exercise" or "varicocele athletes" will return relevant studies.
Google Scholar offers another route to academic literature, often including preprints and conference papers not indexed elsewhere.
The Translational Andrology and Urology journal publishes open-access reviews on male reproductive health topics, including recent comprehensive reviews on varicocele.
When to Seek Urgent Help
While varicocele itself is not an emergency, certain testicular symptoms require immediate medical attention:
Sudden, severe testicular pain—particularly if the testicle appears higher than usual, rotated, or the pain came on very rapidly—could indicate testicular torsion. This is a surgical emergency where blood supply to the testicle is compromised, and delay risks permanent damage. Seek immediate help through A&E or by calling 999.
Testicular pain accompanied by fever, nausea, vomiting, or urinary symptoms may indicate infection (epididymo-orchitis) requiring urgent assessment and treatment.
A new, rapidly growing testicular lump warrants prompt assessment to rule out testicular cancer, which is highly treatable when caught early.
If in doubt about whether your symptoms are urgent, it's always appropriate to seek medical advice. NHS 111 can help you determine the right level of care.
Ready to Discuss Your Situation?
If you'd like to talk through your individual circumstances—whether you're concerned about symptoms affecting your training, have fertility questions, or want to plan treatment around your athletic schedule—I'm available for consultation.
I see patients at Chelsea and Westminster Hospital Private Care, Nuffield Health Highgate Hospital, and via secure video consultation for those who prefer a virtual appointment or are located further afield.
Consultations typically involve a thorough discussion of your history and concerns, clinical examination where appropriate, and a clear plan tailored to your priorities—whether that's optimising training comfort, protecting fertility, or both.

